Table of Contents >> Show >> Hide
- What are tricyclic antidepressants?
- Types of tricyclic antidepressants
- How do tricyclic antidepressants work?
- Main uses of tricyclic antidepressants
- Common side effects of tricyclic antidepressants
- Who should be cautious with tricyclic antidepressants?
- How to use tricyclic antidepressants safely
- When to call your doctor or seek emergency care
- Real-world experiences with tricyclic antidepressants
- The bottom line
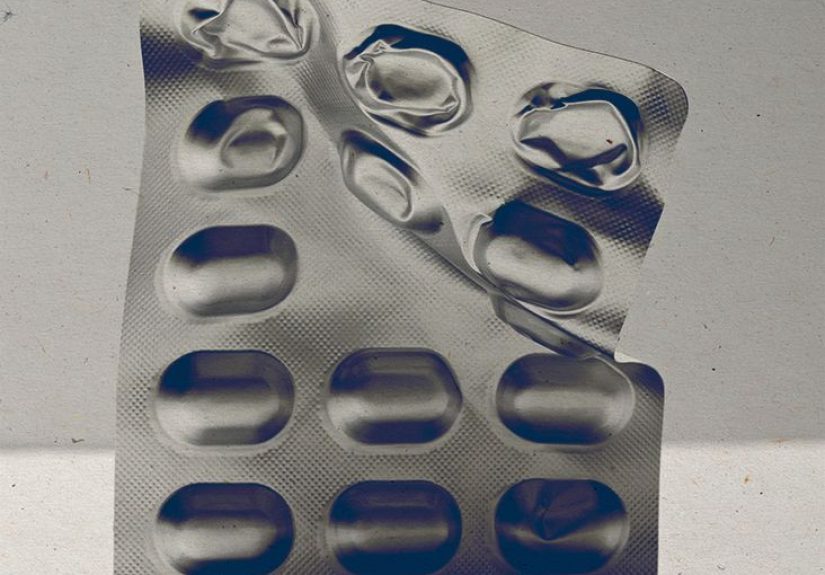
Long before today’s shiny SSRIs and SNRIs took center stage, tricyclic antidepressants (often shortened to TCAs) were the workhorses of depression treatment.
They’re older, a bit rough around the edges, but still incredibly useful when matched to the right person and condition. These medications don’t just help with mood
they can also ease certain types of chronic pain, prevent migraines, and improve sleep when other options fall short.
At the same time, tricyclic antidepressants come with a serious fine print: they can cause bothersome side effects and, in some situations, pose real safety risks.
Understanding the different types of TCAs, how they work, what they’re used for, and their potential downsides can help you have a more informed, confident conversation
with your healthcare provider.
What are tricyclic antidepressants?
Tricyclic antidepressants are a class of prescription medications originally developed to treat major depressive disorder.
Their name comes from their chemical structure: three connected rings (“tri-cyclic”). TCAs work mainly by changing levels of certain brain chemicals,
especially serotonin and norepinephrine, which help regulate mood, pain perception, and sleep.
These drugs were first introduced in the late 1950s and quickly became a mainstay for depression. Today, they’re usually not the first choice for new depression treatment
because newer medications often have milder side effects. However, TCAs still have an important role, especially when:
- Depression hasn’t responded well to other treatments.
- Someone has both depression and chronic pain.
- There’s a specific condition (like migraine or neuropathic pain) where TCAs have strong evidence of benefit.
Types of tricyclic antidepressants
Several tricyclic antidepressants are approved in the United States. Some are used primarily for depression, while others are approved or commonly used for other conditions
like obsessive-compulsive disorder (OCD) or insomnia. Common TCAs include:
TCAs commonly used for depression
- Amitriptyline – Often used for depression, chronic pain, and migraine prevention.
- Imipramine – One of the earliest TCAs, used for depression and sometimes for nighttime bedwetting in children.
- Desipramine – A more “activating” TCA, sometimes preferred in people who feel very slowed down or fatigued.
- Nortriptyline – A “secondary amine” TCA that may cause slightly fewer side effects than some others.
- Doxepin – Used in higher doses for depression and anxiety; very low doses are used as a sleep aid.
- Protriptyline – A more energizing TCA that can help with daytime sleepiness in some cases.
- Trimipramine – Less commonly used, but still part of the TCA family for depression.
Other important TCAs
- Clomipramine – Technically a TCA, but best known for treating obsessive-compulsive disorder (OCD).
- Amoxapine – Another TCA used mainly for depression, with some antipsychotic-like properties.
Although they share a basic structure, different TCAs can feel very different in real life. Some are more sedating, some more stimulating,
and some are more likely to cause specific side effects like weight gain or dry mouth. That’s why picking the “right” one is a job for you and your prescriber,
not a one-size-fits-all decision.
How do tricyclic antidepressants work?
TCAs mainly work by blocking the reuptake (reabsorption) of two key neurotransmitters: serotonin and norepinephrine.
Imagine these chemical messengers as texts sent between brain cells. Normally, after a message is sent, it’s quickly “deleted.”
TCAs slow down that deletion process, leaving more serotonin and norepinephrine available in the brain.
But TCAs don’t stop there. They also interact with other receptors, including:
- Muscarinic (acetylcholine) receptors – Blocking these leads to “anticholinergic” side effects such as dry mouth, constipation, and blurred vision.
- Histamine (H1) receptors – This often causes sedation and weight gain.
- Alpha-1 adrenergic receptors – Blocking these can cause dizziness when standing up (orthostatic hypotension).
These extra actions help explain why TCAs can be very effective for pain and sleepbut also why they can be tough to tolerate and risky in overdose.
Main uses of tricyclic antidepressants
1. Major depressive disorder
TCAs were originally designed to treat major depression, and they’re still effective for this purpose.
They can be especially helpful when other antidepressants haven’t worked, or when someone has a long history of severe or treatment-resistant depression.
Because of their side effect profile and overdose risk, many guidelines now recommend newer medications (like SSRIs and SNRIs) as first-line options.
TCAs often step in later, when:
- Multiple trials of other antidepressants haven’t provided enough relief.
- There’s a strong pain component (for example, fibromyalgia or neuropathic pain alongside depression).
- Someone has previously responded very well to a TCA.
2. Chronic and neuropathic pain
One of the biggest “second careers” for TCAs is chronic pain management. TCAsparticularly amitriptyline and nortriptylineare commonly used for:
- Neuropathic pain (nerve pain), such as pain from diabetes or shingles.
- Fibromyalgia and widespread muscle pain.
- Complex regional pain syndrome.
- Certain types of low back pain.
For chronic pain, TCAs are often prescribed at doses lower than those used for depression. The goal isn’t to knock you outit’s to nudge the nervous system
away from constantly broadcasting “pain!” signals.
3. Migraine and headache prevention
Amitriptyline, in particular, has solid evidence for helping prevent migraines and tension-type headaches. People who get frequent or disabling headaches
may take a low dose of a TCA daily to reduce how often and how severely the headaches strike.
4. Sleep problems and anxiety
Because many TCAs are sedating, they’re sometimes used when insomnia and depression travel together. Doxepin in very low doses is FDA-approved specifically
for sleep maintenance insomnia. TCAs may also help some anxiety disorders, including panic disorder and social anxiety, though they’re less commonly chosen
now that other options exist.
5. Other conditions
Depending on the specific medication, TCAs can play a role in:
- Obsessive-compulsive disorder (clomipramine).
- Nighttime bedwetting (imipramine) in children.
- Functional gastrointestinal disorders, such as irritable bowel syndrome (IBS).
- Bladder pain or overactive bladder symptoms.
- Chronic pelvic pain and certain pelvic floor disorders.
Many of these uses are “off-label,” meaning the FDA hasn’t officially approved the drug for that specific condition, even though research and clinical experience support it.
Your prescriber should explain when a medication is being used off-label and why it might be a good fit for you.
Common side effects of tricyclic antidepressants
Side effects are one of the main reasons TCAs have lost their top billing in depression treatment. Because they interact with several different receptors in the body,
they can cause a wide grab bag of symptoms.
Everyday side effects
Common, often dose-related side effects include:
- Dry mouth – You may feel like you’re constantly thirsty or need sugar-free gum or lozenges.
- Constipation – Due to slowed gut movement from anticholinergic effects.
- Blurred vision – Close-up focusing can be harder, especially at higher doses.
- Drowsiness and fatigue – Often more pronounced with amitriptyline, doxepin, and trimipramine.
- Dizziness or lightheadedness, especially when standing up quickly (orthostatic hypotension).
- Weight gain, partly connected to histamine and appetite changes.
- Sexual side effects, such as decreased desire or difficulty with orgasm.
Some of these effects fade as the body adjusts. Otherslike dry mouth or constipationmay stick around and need lifestyle changes or additional treatments
(for example, more fiber, fluids, or sugar-free candy).
Serious and potentially dangerous side effects
TCAs can also cause less common but more serious problems, especially at higher doses, in overdose, or in people with certain medical conditions. These include:
- Heart rhythm problems – TCAs can affect the electrical conduction system of the heart, leading to changes on an ECG and, rarely, dangerous arrhythmias.
- Low blood pressure and fainting – Severe drops in blood pressure can occur, especially in older adults.
- Confusion, agitation, or delirium – More likely in older people or those with underlying cognitive issues.
- Seizures – High doses or overdose increase this risk.
- Overdose toxicity – A relatively small overdose (about 10–20 mg per kilogram of body weight) can be life-threatening and requires emergency care.
Because of these risks, TCAs are prescribed with particular caution in people with heart disease, seizure disorders, or a history of overdose or suicide attempts.
Mental health and suicidality
Like other antidepressants, TCAs carry a boxed warning about an increased risk of suicidal thoughts and behaviors in children, teens, and young adultsespecially during
the first few weeks of treatment or when the dose is changed. Close monitoring, honest communication about mood changes, and regular follow-up with a mental health
professional are essential.
Who should be cautious with tricyclic antidepressants?
TCAs aren’t a good match for everyone. Your prescriber will typically use extra careor choose another medication entirelyif you have:
- Serious heart disease, recent heart attack, or known heart rhythm abnormalities.
- Untreated narrow-angle glaucoma.
- Significant urinary retention or enlarged prostate.
- Uncontrolled seizure disorder.
- Severe liver disease.
- A history of dangerous overdose or high suicide risk.
TCAs can also interact with other medications, including:
- Monoamine oxidase inhibitors (MAOIs).
- Other drugs that prolong the QT interval on an ECG.
- Some antiarrhythmics, antipsychotics, and antihistamines.
- Other antidepressants or pain medications that increase serotonin, raising the risk of serotonin syndrome.
Always give your healthcare team a full list of everything you takeprescriptions, over-the-counter meds, herbal supplements, and recreational substancesbefore starting a TCA.
How to use tricyclic antidepressants safely
If you and your clinician decide a TCA is worth trying, a few practical habits can make the experience safer and smoother:
- Start low and go slow. TCAs are often started at a low dose and increased gradually to improve tolerability.
- Be patient. For depression and chronic pain, it can take several weeks to notice full benefits.
- Take them exactly as prescribed. Never double up on doses to “catch up” if you miss one.
- Don’t stop suddenly. Abruptly stopping can cause withdrawal-like symptoms or a fast return of depression or pain.
- Keep all follow-up appointments. Your provider may order blood tests or an ECG, especially at higher doses or if you have risk factors.
- Store them safely. Because overdose can be dangerous, keep TCAs away from children, pets, and anyone who might misuse them.
When to call your doctor or seek emergency care
Contact your prescriber promptly if you notice:
- Worsening depression or new suicidal thoughts.
- Severe constipation, trouble urinating, or intense blurred vision.
- Unusual confusion, agitation, or hallucinations.
- Palpitations, chest pain, or feeling like your heart is racing or skipping beats.
Call emergency services or go to the nearest emergency department if you suspect an overdose, experience chest pain, severe difficulty breathing, seizures, or
sudden fainting episodes. Don’t try to manage these symptoms at home.
Real-world experiences with tricyclic antidepressants
Reading about tricyclic antidepressants in a list of side effects is one thing. Seeing how they play out in real life is another.
Experiences vary widely from person to person, but a few common themes pop up again and again in clinic visits and patient stories.
Finding relief when newer options fail
Consider someone who has tried multiple modern antidepressants with only partial relief. They’re exhausted, discouraged, and wondering if anything will work.
When a TCA like nortriptyline is added thoughtfullystarting at a low dose, with close monitoringit can sometimes provide that extra nudge that finally moves mood
from “barely coping” to “actually living again.” The trade-off might be dry mouth and the need for more frequent dental care, but for some, the mood improvement is worth it.
Healthcare providers often describe TCAs as “powerful but demanding” tools: they’re not right for everyone, but when they fit, they can make a meaningful difference.
Turning down the volume on chronic pain
People with neuropathic painlike burning, tingling, or electric shock–type pain from diabetes or shinglessometimes describe TCAs as turning down the “pain volume.”
The pain may not disappear completely, but instead of shouting at a 10 all day, it drops to a more manageable 4 or 5.
This kind of relief can translate into better sleep, more social activity, and a greater ability to work or enjoy hobbies. At the same time,
those same people often have to juggle side effects: perhaps taking the medication only at night to minimize daytime drowsiness, working with their provider to
tweak the dose, or switching from one TCA to another in search of a better balance.
Managing migraines and reclaiming routines
For someone with frequent migraines, a low-dose TCA may feel like getting part of their life back. Instead of multiple attacks every week, they might drop to one or two
per monthor even less. That can mean fewer missed workdays, fewer last-minute cancellations, and fewer afternoons spent hiding in a dark room.
On the flip side, starting a TCA for migraine prevention often brings a short “adjustment period” where fatigue is more noticeable. Patients sometimes describe needing
an extra week or two to figure out the best time to take the medication (usually in the evening) and to accept that bedtime might need to come a bit earlier.
The importance of personalization and partnership
One of the biggest lessons from real-world use is that TCAs are most effective when the person taking them feels like a true partner in the process.
That includes being honest about side effects, asking questions about long-term risks, and speaking up if something doesn’t feel right.
Some people decide that the trade-offs are worth it; others try a TCA briefly and then move on to a different option. Neither path is “wrong.”
The goal isn’t to force your life to fit a particular medicationit’s to find a treatment plan that fits your life, values, and health priorities.
If you’re considering a tricyclic antidepressant, it’s perfectly reasonable to ask your clinician:
- Why this specific TCA instead of another antidepressant?
- What benefits are we hoping for in my particular situation?
- What early side effects should I expect, and which ones would be red flags?
- How will we decide whether to stay on it, change the dose, or switch?
TCAs are not “good” or “bad” in themselvesthey’re tools. With the right information, careful dosing, and ongoing follow-up, they can still play a valuable role
in modern mental health and pain management.
The bottom line
Tricyclic antidepressants are older medications, but they haven’t become irrelevant. They remain powerful options for certain people with depression,
chronic pain, migraines, and other conditionsespecially when newer drugs haven’t delivered the hoped-for results. At the same time, their side effects and overdose risk
demand respect, careful monitoring, and an honest conversation about benefits versus downsides.
If you’re thinking about starting, stopping, or changing a TCA, always talk with a healthcare professional who knows your full medical story.
Online information (including this article) can guide your questionsbut it’s not a substitute for personalized medical advice.