Table of Contents >> Show >> Hide
- What a Lung PET Scan Is (and What It Isn’t)
- Purpose: Why Doctors Order a Lung PET Scan
- How Accurate Is a Lung PET Scan?
- Procedure: What Happens During a Lung PET Scan
- Preparation: How to Get Ready (Without Overthinking It)
- What the Results Mean (In Plain English)
- Risks and Safety: Should You Be Worried?
- FAQ: Quick Answers to Common Questions
- Patient Experiences: What It’s Really Like (500+ Words)
- The day before: the “low-carb scavenger hunt”
- Scan morning: fasting, but make it practical
- Check-in and the IV: the most dramatic two minutes
- The uptake period: quiet time that feels louder than it is
- In the scanner: “I thought it would be worse”
- Afterward: water, bathroom breaks, and the waiting game
- Final Thoughts
A lung PET scan can sound like something from a sci-fi movie (“We’re going to scan your cells for suspicious behavior.”),
but it’s actually a very practical, widely used imaging test. PET stands for positron emission tomography,
and it helps doctors see how active certain tissues areespecially when they’re looking for cancer, checking how treatment is working,
or investigating a suspicious lung spot that won’t stop being mysterious.
Unlike a regular chest X-ray or CT scan that focuses mainly on structure (what things look like),
a PET scan focuses on function (what things are doing). Many lung PET scans are done as a combined
PET/CT, which pairs “activity” data from PET with the detailed anatomy from CT.
What a Lung PET Scan Is (and What It Isn’t)
Most lung PET scans use a tracer called FDG (fluorodeoxyglucose), a form of glucose (sugar) tagged with a tiny amount
of radioactive material. Since many cancers use glucose more aggressively than normal tissue, FDG can highlight areas that are unusually
“hungry,” which may suggest cancer or other high-activity processes.
Important: PET doesn’t automatically mean “cancer detector.” Inflammation and infection can also show increased FDG uptake.
PET is a powerful clue generatornot a final verdict.
PET vs. CT vs. PET/CT
- CT scan: Great at showing detailed structuresize, shape, location, and anatomy.
- PET scan: Shows metabolic activityhow actively cells are taking up the tracer.
- PET/CT: Combines both, helping pinpoint where the activity is happening and what it corresponds to anatomically.
Purpose: Why Doctors Order a Lung PET Scan
A lung PET scan is often ordered when your care team needs more information than a CT alone can provideespecially when the question is
“Is this suspicious spot active in a way that suggests cancer, and if so, where else might it be?”
Common reasons include:
- Evaluating a pulmonary nodule or lung mass: If a CT finds a lump or nodule, PET may help determine whether it’s metabolically active.
- Lung cancer staging: PET/CT can help check if cancer has spread to lymph nodes or other parts of the body.
- Treatment planning: The scan can guide decisions about surgery, radiation, chemotherapy, immunotherapy, or combinations of these.
- Checking response to treatment: PET can show whether a tumor’s activity is decreasing, sometimes before it changes in size.
- Looking for recurrence: If symptoms return or follow-up scans raise questions, PET may help identify active disease.
-
Clarifying confusing findings: Scar tissue, atelectasis (collapsed lung areas), and post-treatment changes can look suspicious on CT.
PET may help sort out what’s active vs. what’s just “old news.”
Specific example: “A suspicious lung nodule”
Imagine a CT shows an 11 mm nodule in the upper lobe. That’s big enough to care about, but not big enough to instantly explain itself.
A PET/CT can evaluate FDG uptake in that nodule and also scan the rest of the body for other areas of concern, which matters if your team is
deciding between watchful waiting, biopsy, or surgery.
How Accurate Is a Lung PET Scan?
PET/CT is very helpful, but it’s not perfect. Accuracy depends on the size of the lesion, the tumor type, your blood sugar level,
and whether infection or inflammation is present.
Why PET can miss things (false negatives)
- Small lesions: Very small nodules may not show strong uptake due to scanner resolution limits.
- Slow-growing or low-metabolic tumors: Some cancers just don’t “light up” much on FDG PET.
- High blood glucose: If your blood sugar is high, FDG distribution can be less reliable (your body is literally competing with the tracer).
Why PET can “overcall” things (false positives)
- Infection or inflammation: Pneumonia, TB, fungal infections, sarcoidosis, and other inflammatory conditions can increase FDG uptake.
- Healing tissues: Recent surgery, biopsy, or radiation can cause temporary inflammatory uptake.
Bottom line: PET helps refine the probability of disease and guides next steps (biopsy, follow-up imaging, treatment decisions),
but diagnosis often still relies on pathology (biopsy) when needed.
Procedure: What Happens During a Lung PET Scan
The process is usually straightforward. The hardest part for many people is the waiting (and not the “I’m bored” waitingthe “I hope my results are okay” waiting).
Here’s the typical flow:
1) Check-in and screening
- You’ll confirm your medical history, medications, allergies, and whether you could be pregnant or breastfeeding.
- You may change into a gown and remove metal items (zippers, jewelry, certain underwire brasyes, the scan is picky).
- Your care team may check your blood glucose before giving the tracer, especially for FDG PET scans.
2) IV placement and tracer injection (FDG)
A technologist places an IV line and injects the tracer. The amount of radioactivity is small and designed to decay quickly.
Most people feel little to nothing from the injection itself, aside from the standard IV “hello, needle” moment.
3) Uptake period (quiet resting time)
After injection, you’ll rest quietly while the tracer circulates and is taken up by tissues. This is typically around
45 to 60 minutes. During this time:
- You’ll likely be asked to stay still and relaxed.
- Talking, chewing, or moving a lot can increase muscle uptake and potentially affect image quality.
- You may be encouraged to drink water (unless instructed otherwise).
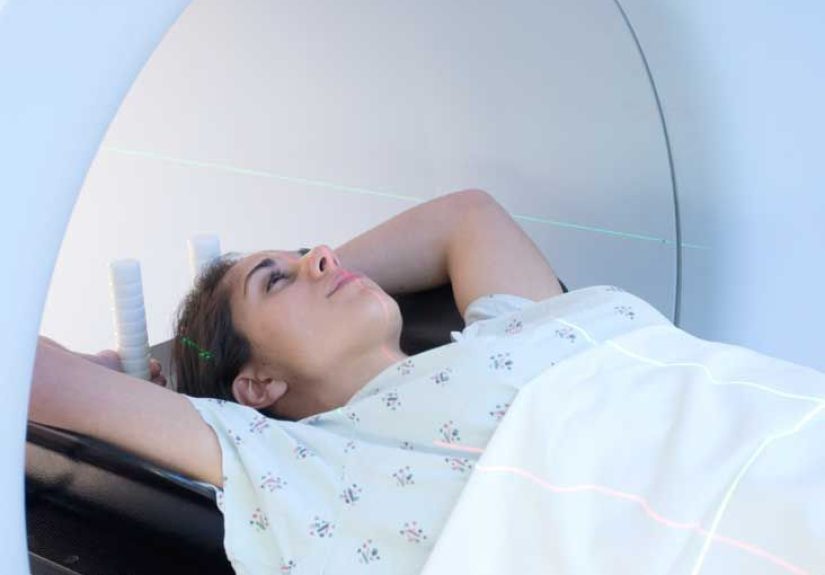
4) The scan itself
You’ll lie on a padded table that slides through the scanner. PET/CT scanners are open at both ends and not as confining as some MRI machines,
but if you dislike tight spaces, tell your team ahead of time.
- Duration: The scanning portion often takes about 20–40 minutes, depending on protocol.
- What you do: Lie still and breathe normally unless told otherwise.
- Sounds: Expect humming/clicking; it’s the machine doing its job, not judging you.
5) After the scan
Once the images are done, you can usually go home the same day. You’ll be advised to drink plenty of fluids and urinate frequently to help clear the tracer.
Your provider will tell you when to expect resultsoften within a day or two, sometimes sooner depending on the facility.
Preparation: How to Get Ready (Without Overthinking It)
Preparation matters because FDG behaves like glucose. If you eat right before the scan, your body routes sugar to muscles and other tissues,
and the tracer distribution can be less useful. Follow your facility’s instructions exactly, but these are common guidelines.
Food and drink
- Fasting: Many centers ask you to stop eating for 4–6 hours before the tracer injection. Water is usually allowed.
- Skip sugar and calories: Avoid juice, soda, sweet tea, energy drinks, and even “just a little creamer.”
- Low-carb guidance: Some facilities recommend a low-carbohydrate diet for 24 hours before the scan to reduce background uptake.
Exercise and activity
- Avoid strenuous exercise: Often for 24–48 hours beforehand. Heavy exercise can increase muscle uptake and muddy the images.
- Stay warm: Being cold can activate brown fat, which can show FDG uptake and make interpretation harder. Dress comfortably.
Medications and diabetes considerations
Always follow your ordering team’s instructions about medications. If you have diabetes, you may receive a customized plan to balance fasting,
blood sugar control, and accurate imaging. This might include timing adjustments for insulin or other meds and specific meal timing.
Pregnancy and breastfeeding
- Pregnancy: Tell your provider if you’re pregnant or might be. PET/CT involves radiation, and your team will weigh risks and benefits.
- Breastfeeding: You may be instructed to pause breastfeeding for a period after the tracer, depending on the tracer used and facility protocol.
What to bring and wear
- Wear comfortable clothing without metal when possible (or expect to change into a gown).
- Bring your medication list and any relevant imaging history if requested.
- If you’re claustrophobic, ask ahead about anxiety medication options and whether you’ll need a ride home.
What the Results Mean (In Plain English)
PET results are interpreted by a radiologist or nuclear medicine physician. They look for areas of increased tracer uptake
and compare them to normal patterns. They also correlate findings with CT anatomy.
SUV: The number you may hear about
You might see the term SUV (standardized uptake value). It’s a semi-quantitative measure of how much tracer a region takes up.
Higher SUV can be associated with malignancy, but it’s not a magic “cancer number.” SUV depends on many variables, and interpretation is always
done in clinical context.
Common PET/CT result scenarios
- Low uptake in a small nodule: Often reassuring, but may still need follow-up imaging depending on risk and size.
- High uptake in a lung mass: Raises concern and may lead to biopsy, staging workup, or treatment planning.
- Uptake in lymph nodes: Can suggest spreadbut could also reflect inflammation, so context matters.
- Unexpected uptake elsewhere: Sometimes PET finds unrelated issues that require follow-up (not always serious, but worth checking).
Risks and Safety: Should You Be Worried?
For most people, a lung PET scan is safe and well-tolerated. The main considerations are radiation exposure and special situations
such as pregnancy or certain medical conditions.
Potential risks
- Radiation exposure: PET (tracer) plus CT (if PET/CT) adds exposure. The benefit is improved diagnosis and treatment planning.
- Allergic reaction: Rare with FDG tracer. If contrast is used for the CT portion, contrast allergy risks may apply.
- IV-related issues: Minor bruising or discomfort at the injection site.
If you’re anxious, it’s okay to say so. Anxiety is common, and imaging departments deal with it every day. You’re not the first person to ask,
“Can I bring a stress ball?” (You can ask. They’ll probably say yes, as long as it doesn’t interfere with scanning.)
FAQ: Quick Answers to Common Questions
How long does a lung PET scan take?
Plan on being there about 2 hours (sometimes 2–3). The uptake period is often the longest part. The scan itself may take under an hour.
Does it hurt?
The scan is painless. The IV placement may sting briefly. The rest is mainly “lie still and let the machine do its thing.”
Can I drive myself home?
Usually yesunless you take a sedative for anxiety. If you do, you’ll likely need someone else to drive.
Will I be radioactive afterward?
You’ll have a small amount of radioactivity that decays quickly. Most centers advise hydration and normal precautions,
and some may recommend limiting close contact with infants or pregnant individuals for a short time.
Patient Experiences: What It’s Really Like (500+ Words)
Let’s talk about the part brochures don’t fully capture: the lived experience. People usually don’t fear the scanner as much as they fear
what the scanner might reveal. The emotional side is realand it’s normal.
The day before: the “low-carb scavenger hunt”
If your imaging center asks for a low-carb day, it can feel like you’re suddenly reading nutrition labels like a detective:
“This yogurt has how much sugar?” Many people keep it simpleeggs, chicken, fish, tofu, leafy greens, and plenty of water.
The goal isn’t a trendy diet makeover; it’s a short-term strategy to help your images come out clearer.
A common tip people share: don’t experiment with a brand-new spicy dinner the night before. Not because it ruins PET scans,
but because spending your scan day with heartburn is an optional side quest.
Scan morning: fasting, but make it practical
Fasting is usually the biggest annoyance. People describe it as “I wasn’t even hungry until you told me not to eat.”
Some bring a snack for afterwardsomething easy like crackers, a sandwich, or a protein barespecially if they have a drive home.
If you’re diabetic, many patients say the best thing they did was call ahead early to confirm medication timing,
so there were no surprises at check-in.
Check-in and the IV: the most dramatic two minutes
The scan itself is calm, but the IV can be the moment that spikes nerves. Most people report it’s quick and manageable.
If you’re someone whose veins like to play hide-and-seek, hydrating beforehand (as allowed) can help. Many imaging centers are pros
at IV placementthis is their daily routine, not an occasional hobby.
The uptake period: quiet time that feels louder than it is
After FDG injection, you rest. This is where many people realize they weren’t prepared for the mental part: sitting still with your thoughts.
Some centers keep the room dim and quiet. People often say they wished they’d brought:
- a warm hoodie or blanket (cold rooms happen),
- something calming like a short meditation track (if allowed),
- or a plan for what they’ll do after the scansomething normal and grounding.
Many centers limit talking and movement during uptake for image quality, which can feel strange, like you’re training to be a museum statue.
But it’s temporaryand it has a purpose.
In the scanner: “I thought it would be worse”
A very common experience: people expect the scanner to feel claustrophobic, but then realize it’s more open than they imagined.
The table moves, the machine makes noises, and you focus on staying still. If you’re anxious, some patients use simple techniques:
slow breathing, counting breaths, or imagining a playlist in their head. (Bonus: you can’t forget lyrics you don’t know.)
Afterward: water, bathroom breaks, and the waiting game
After the scan, most people feel physically fine. The practical advice is consistent: drink water and expect a few extra bathroom trips.
Emotionally, though, many people describe the next 24–48 hours as the hardest partwaiting for results.
What helps? Patients often say they felt better when they reminded themselves of two truths:
(1) a PET scan is information, and information helps your team make better decisions; and
(2) results usually need expert interpretationso “don’t Google every sentence in your report at 2 a.m.” is genuinely good life advice.
If you do read your report, write down questions and review them with your doctor, who can explain what findings mean in your specific situation.
Final Thoughts
A lung PET scan is a powerful tool for understanding what’s happening in the lungs and beyondespecially for evaluating suspicious findings,
staging lung cancer, and assessing response to treatment. The best way to set yourself up for a smooth scan is to follow prep instructions closely,
communicate clearly about diabetes or pregnancy/breastfeeding, and plan something comforting for afterward. The scanner’s job is to collect data;
your care team’s job is to turn that data into a plan.







