Table of Contents >> Show >> Hide
- What Is Adenomyosis?
- Adenomyosis Symptoms
- Why Does Adenomyosis Happen?
- Adenomyosis Diagnosis
- Adenomyosis Treatments
- Day-to-Day Strategies That Can Make Symptoms More Livable
- How to Advocate for Yourself at Appointments
- FAQs
- Real-Life Experiences: What People Often Describe (and What Helps)
- Final Takeaway
If your uterus had a customer service desk, adenomyosis would be the complaint ticket that reads:
“Hi, I’d like to be lined with endometrial tissue… AND also have that tissue show up in the muscle wall.
Thanks!” Unfortunately, the uterus is an overachiever with no off switch, and adenomyosis can turn
regular periods into a monthly event with VIP seating, extra confetti (blood), and a soundtrack of cramps.
The good news: adenomyosis is benign (not cancer). The also-true news: it can be painful,
exhausting, and confusingespecially because its symptoms overlap with fibroids, endometriosis, and other
causes of abnormal uterine bleeding. This guide breaks down what adenomyosis is, what it feels like, how
doctors diagnose it, and the treatments that can actually help.
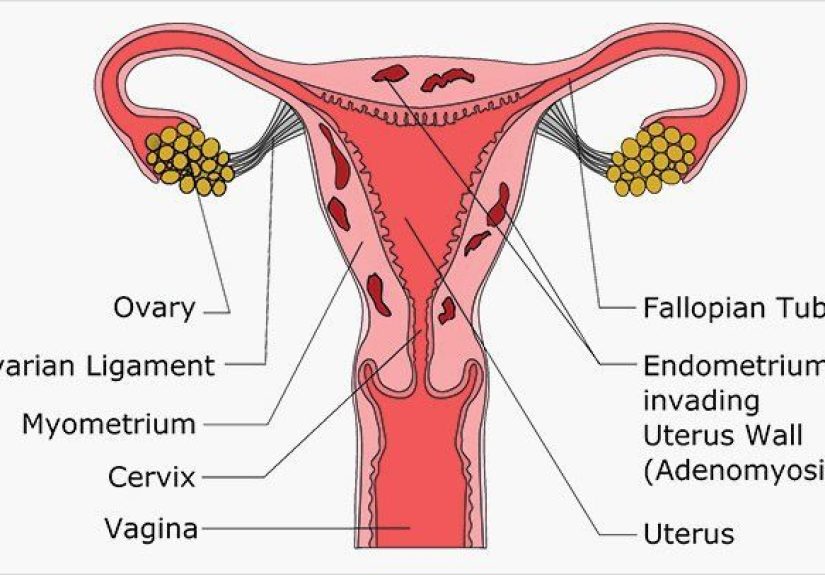
What Is Adenomyosis?
Adenomyosis happens when tissue similar to the uterine lining (endometrium) grows into the
muscular wall of the uterus (myometrium). That tissue still responds to monthly hormonesthickening,
breaking down, and bleedingexcept now it’s embedded where it can irritate muscle, trigger inflammation,
and contribute to a uterus that becomes enlarged or “boggy” on exam.
Adenomyosis vs. Fibroids vs. Endometriosis
-
Fibroids are noncancerous muscle tumors that form distinct “lumps.”
Adenomyosis is more like tissue scattered or blended within the uterine muscle. -
Endometriosis is endometrial-like tissue growing outside the uterus (like on ovaries or pelvic lining).
Adenomyosis is inside the uterusspecifically, inside the uterine wall. - You can have more than one of these at the same time, which is one reason diagnosis can take a while.
Adenomyosis Symptoms
Some people have adenomyosis and feel basically fine (rude, but true). Others have symptoms that
disrupt school, work, and quality of life. Symptoms often show up in the later reproductive years,
but improved imaging is helping clinicians recognize adenomyosis in younger patients too.
1) Heavy or Prolonged Periods
A common sign is heavy menstrual bleedingsometimes with periods that last longer than usual,
frequent pad/tampon changes, or bleeding that causes anemia (low iron). Many people describe feeling
drained, foggy, or short of breath during their cycle because the body is basically running a “blood donation
program” it never signed up for.
2) Painful Periods (Dysmenorrhea)
Adenomyosis can cause strong cramps that worsen over time. Some people notice pain starts earlier
before the period, lasts longer, or radiates to the back and thighs. Heat packs become a personality trait.
3) Pelvic Pressure, Bloating, or a “Heavy” Feeling
Because the uterus may enlarge, some people feel pelvic pressure or a sensation of fullnesssimilar to
what fibroids can cause. Not everyone gets visible belly changes, but the “why do my jeans hate me today?”
feeling can be real.
4) Pain During Sex or Chronic Pelvic Pain
Some people experience pain during sex or ongoing pelvic discomfort. If this is happening, it’s a
legitimate medical issuenot something you should be told to “just relax” through. (If relaxing cured
gynecologic pain, the world would be very different.)
When to Seek Care Quickly
Get urgent medical attention if you have very heavy bleeding (for example, soaking through protection very
quickly), feel faint, have chest pain, severe weakness, or signs of significant anemia. You don’t need to “earn”
care by suffering longer.
Why Does Adenomyosis Happen?
Experts don’t fully agree on one single cause. Leading theories include the uterine lining pushing or
“invaginating” into the muscle layer, tissue changes after pregnancy, or changes after uterine procedures.
What’s clear is that adenomyosis is hormone-responsive, which is one reason symptoms often improve
after menopause.
Common Risk Factors
- Age: many diagnoses occur in the 40s and 50s (though not exclusively).
- Prior pregnancies (parity) are associated with increased risk in multiple reviews.
- History of uterine procedures (like C-section, D&C, or other uterine surgery) may increase risk.
Adenomyosis Diagnosis
Adenomyosis used to be confirmed mostly after hysterectomy, when tissue could be examined under a microscope.
Today, clinicians can often make a diagnosis without removing anythingthanks to better imaging and clearer
diagnostic criteria.
Step 1: Symptoms + Medical History
Your clinician will ask about bleeding patterns, pain timing, past pregnancies, prior procedures, and whether
symptoms have changed over time. Tracking your cycle for 1–2 months (even quick notes on your phone) can help:
start date, duration, pain days, bleeding heaviness, and how often you need medication.
Step 2: Pelvic Exam
On exam, adenomyosis may be associated with a uterus that feels enlarged, tender,
or diffusely “boggy.” This isn’t definitive by itself, but it raises suspicionespecially when paired with
heavy bleeding and painful periods.
Step 3: Imaging (Usually Transvaginal Ultrasound First)
Transvaginal ultrasound is commonly the first imaging test used. It can show features suggestive of
adenomyosis, such as changes in the uterine muscle texture or signs that the boundary between layers is less
distinct than usual. Ultrasound is widely available, fast, and often the best starting point.
If the ultrasound is unclearor if symptoms are complexyour clinician may recommend
MRI. MRI can provide more detailed images of the uterine wall and may help in “equivocal” cases
where the diagnosis is uncertain.
Step 4: Ruling Out Look-Alikes
Adenomyosis can mimic fibroids and can also exist alongside them. Your clinician may also evaluate for
thyroid disorders, bleeding disorders, polyps, endometriosis, or other causes of pelvic pain and abnormal
uterine bleeding. A good workup is less “let’s run every test ever” and more “let’s be strategic and not miss
something fixable.”
Adenomyosis Treatments
Treatment depends on your symptoms, age, overall health, and whether you want to preserve fertility.
The goal is usually one (or more) of these: reduce bleeding, control pain,
improve daily function, andwhen relevantsupport pregnancy goals.
1) Anti-Inflammatory Pain Relief (NSAIDs)
Many clinicians recommend NSAIDs (like ibuprofen or naproxen) to reduce cramps and inflammation.
Some people get better results when they start NSAIDs 1–2 days before bleeding begins and continue during
the heaviest days (if medically safe for them). If you have stomach ulcers, kidney disease, or are on certain
medications, NSAIDs may not be appropriateso this is one to personalize.
2) Hormonal Treatments to Reduce Bleeding and Pain
Because adenomyosis is hormone-responsive, many first-line therapies focus on
hormonal menstrual suppressionbasically turning down the monthly “build-and-shed” cycle.
-
Levonorgestrel-releasing IUD (a progestin IUD): often used to reduce heavy bleeding and cramping.
Many people like it because it targets the uterus directly and can be long-acting. - Combined hormonal birth control (pill/patch/ring): can regulate cycles and reduce bleeding and pain.
- Progestin-only options (pills, injections, implants): may help when estrogen isn’t advised.
-
GnRH agonists/antagonists (short-term use in selected cases): create a low-estrogen state that can
reduce symptoms, sometimes used as a bridge before procedures or surgery.
Hormonal treatments are not one-size-fits-all. Side effects vary, and the “best” choice depends on migraine
history, blood clot risk, mood sensitivity, and your fertility timeline. If a medication makes you feel like
a different person (and not in a fun superhero way), tell your clinicianthere are alternatives.
3) Non-Surgical Procedures (Uterus-Preserving Options)
If symptoms aren’t controlled with medicationor if medication isn’t a good fitsome people consider
procedures designed to reduce bleeding and pain while keeping the uterus.
-
Uterine artery embolization (UAE): performed by interventional radiology to reduce blood supply
to uterine tissue. UAE is better known for fibroids but may also help selected adenomyosis cases.
It isn’t ideal for everyone, and pregnancy after UAE is generally approached cautiouslyso this is a
“talk in detail with your specialist” option. -
Endometrial ablation: removes/destroys the uterine lining to reduce bleeding. It may not address
adenomyosis deep in the uterine wall and is not recommended for those planning pregnancy. -
Conservative surgery (adenomyomectomy in selected cases): removal of localized adenomyosis
tissue can be considered in specialized settings, particularly when fertility preservation is important.
This is complex and depends on disease pattern and surgeon experience.
4) Hysterectomy (Definitive Treatment)
Hysterectomy (removal of the uterus) is the only consistently “definitive” cure for adenomyosis,
because the disease is inside the uterine wall. It’s typically considered when symptoms are severe,
other treatments have failed, and future pregnancy isn’t desired.
Choosing hysterectomy isn’t “giving up.” It can be a thoughtful, quality-of-life decisionespecially for people
who have spent years planning their lives around pain, bleeding, and fatigue.
What About Fertility and Pregnancy?
Adenomyosis has been associated with difficulty conceiving and may be linked to certain pregnancy
complications in some studies, but individual outcomes vary widely. If you’re trying to conceive and have
symptoms like heavy bleeding or significant period pain, it’s reasonable to ask for evaluation sooner rather
than later. Some treatments (like certain hormonal therapies) prevent pregnancy while used, so fertility goals
should be part of the plan from day one.
Day-to-Day Strategies That Can Make Symptoms More Livable
Lifestyle changes won’t “cure” adenomyosis, but they can reduce the amount of suffering stacked on top of the
condition (which matters a lot).
- Heat therapy: heating pads and warm baths can relax muscle and reduce cramping.
- Movement: gentle walking, stretching, yoga, or low-impact exercise may help some people.
- Iron support: if heavy bleeding is an issue, ask about iron testing and replacement.
- Sleep and stress support: pain is louder when you’re exhausted; protect your rest when you can.
- Pelvic floor physical therapy: can be helpful when chronic pelvic pain leads to muscle tension.
How to Advocate for Yourself at Appointments
You don’t need a medical degree to deserve a clear plan. Here’s a simple way to show up prepared:
Track These for 1–2 Cycles
- Days of bleeding and how heavy it is (light/medium/heavy)
- Worst pain level (0–10) and which days it happens
- Medication used and whether it helped
- Fatigue, dizziness, or shortness of breath (possible anemia clues)
- Any missed school/work or canceled activities
Questions Worth Asking
- “Based on my symptoms and exam, what diagnoses are you considering?”
- “Should I get a transvaginal ultrasound, MRI, or both?”
- “What’s the first-line treatment plan, and what’s plan B if this doesn’t work?”
- “How does this plan change if I want children in the future?”
- “Should we check my iron or screen for anemia?”
FAQs
Is adenomyosis dangerous?
It’s usually not dangerous in a life-threatening sense, but it can be life-disrupting. Heavy bleeding can lead
to anemia, and ongoing pain can affect sleep, mood, relationships, and productivity.
Does adenomyosis go away after menopause?
Symptoms often improve after menopause, likely because the condition is hormone-responsive. That said,
you shouldn’t have to wait years for relief if symptoms are severe now.
Can adenomyosis be cured without surgery?
Many people manage symptoms well with medication or uterus-preserving procedures, but hysterectomy is
generally considered the definitive cure because it removes the organ where adenomyosis lives.
Can I have adenomyosis and fibroids together?
Yes, and it’s common for symptoms to overlap. That’s one reason imaging and a careful evaluation matter.
Real-Life Experiences: What People Often Describe (and What Helps)
Adenomyosis doesn’t come with a flashing neon sign. For many people, it shows up as a slow pattern:
“My periods are getting heavier,” “cramps are getting worse,” and “I’m more tired than I should be.”
One common experience is realizing that your personal calendar has quietly been replaced by your uterus’s
calendar. Plans get made with a mental footnote: Unless it’s one of those weeks.
A lot of people describe the early stage as confusing rather than dramatic. They try a new brand of pads,
add a hot water bottle, assume stress is making things worse, and push through. Then they notice the pain
lasts longer each month or the bleeding becomes unpredictable. Some end up in a cycle of “normal test results”
that don’t match how they feel. When ultrasound finally suggests adenomyosis, the reaction is often a mix of
relief (“It’s not all in my head”) and annoyance (“So I wasn’t imagining it… cool cool cool.”).
Another common experience: trial-and-error treatment. Someone might start with NSAIDs and find
they help a littleenough to get through class or work, but not enough to feel normal. Then they try hormonal
birth control and discover it’s a lifesaver, or… it makes them feel emotionally upside down, so they switch.
People who do well often describe success as a combination of the right medication plus small supports:
keeping a heating pad at home, planning lower-stress days during the heaviest bleeding, and treating iron
deficiency when it shows up.
For those who choose a levonorgestrel IUD, experiences vary. Some people say bleeding lightens significantly
and cramps calm down over time, while others need additional strategies (or decide it’s not the right fit).
What tends to help emotionally is having a clinician set expectations honestly: “This may take a few months
to judge,” and “If it’s not working, we’ll move to the next option.” That kind of clarity turns the process
from “I’m stuck like this forever” into “We’re testing solutions, one step at a time.”
People considering procedureslike uterine artery embolizationoften describe a different kind of stress:
decision fatigue. They’re weighing symptom relief against recovery time, cost, and fertility goals. Many say
it helps to bring a written list of priorities to appointments. For example: “My top goal is stopping heavy
bleeding,” or “I need pain control without stopping ovulation,” or “Preserving fertility is non-negotiable.”
Turning vague suffering into specific goals makes treatment discussions clearer and less overwhelming.
And for people who choose hysterectomy, the most common reflection is not regretit’s relief.
They often describe realizing how much energy they spent coping: packing extra supplies, mapping bathrooms,
canceling events, and bracing for pain. After recovery, many say they wish they’d been offered a fuller,
earlier conversation about all optionsnot because surgery is always the answer, but because feeling informed
is powerful. In the end, the “best” adenomyosis treatment is the one that gives you your life backwhether
that’s medication, a procedure, or surgerywithout requiring you to be a hero every month.
Final Takeaway
Adenomyosis is a common, often underrecognized cause of heavy periods and pelvic pain. Diagnosis usually
starts with symptoms and exam, then is supported by transvaginal ultrasound and sometimes MRI. Treatment
ranges from anti-inflammatory medication and hormonal therapies (including progestin IUDs) to uterus-preserving
procedures and, for some, hysterectomy as a definitive cure. If your periods are changing, getting heavier,
or hurting more than they used to, you’re not being “dramatic”you’re noticing data. Bring that data to a
clinician who listens, and build a plan that matches your goals.







