Table of Contents >> Show >> Hide
- First: What emphysema prevention really means
- Big risk factors: Who should be extra serious about prevention?
- Tip #1: Don’t smokeand if you do, make quitting your #1 lung project
- Tip #2: Dodge lung irritants like they’re spoilers for your favorite show
- Tip #3: Prevent respiratory infections (they can speed up lung decline)
- Tip #4: Build lung reserve with movement (yes, even if you hate cardio)
- Tip #5: Eat and sleep like your lungs are on your team (because they are)
- Tip #6: Know your riskespecially the genetic “plot twist” (alpha-1)
- Tip #7: Get symptoms checked early (because “it’s probably nothing” is not a plan)
- Common myths (let’s retire these)
- A quick emphysema prevention checklist
- Bottom line
- Experiences: What emphysema prevention looks like in real life (about )
- SEO Tags
If lungs had an instruction manual, the first page would say: “Please do not fill with smoke, dust, or mystery fumes.”
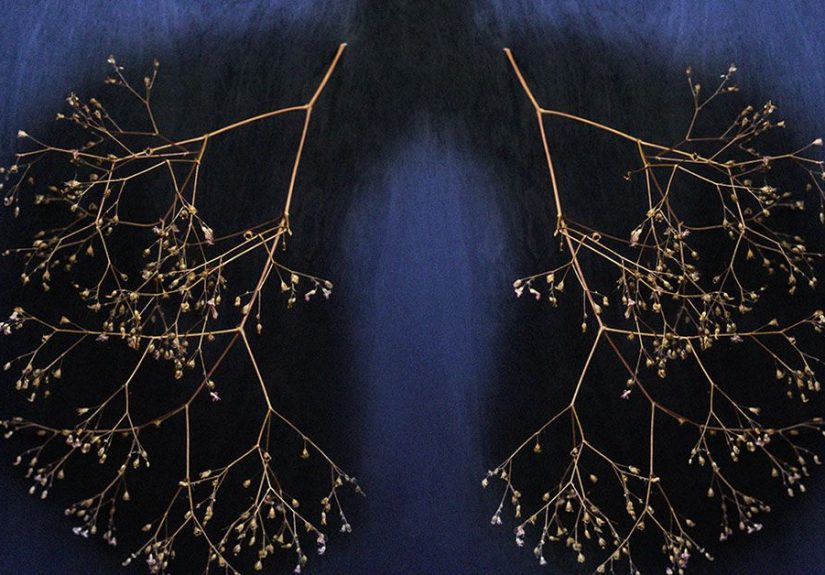
Emphysema is a type of COPD (chronic obstructive pulmonary disease) that damages the tiny air sacs (alveoli) where oxygen exchange happens.
Once those air sacs are injured, you can’t “undo” the damagebut you can prevent emphysema from developing in the first place and slow it down if early changes have started.
This guide breaks down emphysema prevention into practical, real-world steps (no guilt trips, no lecture voice), with specific examples and habits you can actually keep.
The theme is simple: reduce lung irritants, cut your exposure to “lung enemies,” and stack small wins that add up to long-term lung health.
First: What emphysema prevention really means
Prevention has two layers:
- Primary prevention: keeping emphysema from startingespecially by avoiding tobacco smoke and other chronic irritants.
- Progression prevention: slowing further lung damage if you’re already at risk (past smoking, workplace exposure, asthma, family history, or early COPD changes).
Think of it like protecting a favorite white T-shirt. You can avoid ketchup entirely (primary prevention), and if ketchup already happened, you can still stop rubbing it in (progression prevention).
Either way, your future self will thank you.
Big risk factors: Who should be extra serious about prevention?
Emphysema can affect anyone, but your risk goes up if you’ve had long-term exposure to irritantsespecially tobacco smoke.
Other factors include secondhand smoke, air pollution, chemical fumes, dust, and certain workplace exposures.
Genetics can also matter, particularly with alpha-1 antitrypsin deficiency (more on that soon).
Watch-outs that deserve a “let’s protect these lungs” plan
- Current or past cigarette smoking (including heavy secondhand exposure)
- Regular exposure to dust, fumes, or chemicals at work (construction, manufacturing, mining, welding, woodworking, agriculture, salons, auto shops)
- Frequent respiratory infections or chronic cough/wheeze
- Living in areas with high air pollution or wildfire smoke seasons
- Family history of COPD/emphysema or early breathing problems
Tip #1: Don’t smokeand if you do, make quitting your #1 lung project
This is the main event. Smoking is the biggest preventable cause of emphysema.
If you never start, you’re doing the single strongest emphysema prevention move available.
If you already smoke, quitting is still the most powerful step to protect your lungs going forwardno matter how long you’ve smoked.
A quit plan that works in real life (not just in motivational posters)
- Pick a quit date (soon, not “someday”). Give yourself time to prepare, but don’t let it turn into a forever project.
- List your triggers (stress, driving, after meals, certain friends, late-night scrolling) and plan swaps for each.
- Choose your support: coaching, quitlines, text programs, apps, or counseling. Quitting is hard; doing it alone is optional.
- Consider evidence-based tools like nicotine replacement therapy (patch, gum, lozenge) or prescription optionsespecially if cravings hit like a freight train.
- Make your environment boring for smoking: remove cigarettes/lighters, clean fabrics, change routines, and avoid “smoke zones.”
Quick reality check: cravings usually peak and pass like a wave.
The goal isn’t “never crave”it’s “ride the wave without smoking.”
A trick many people like is the 3-minute delay: set a timer, drink water, move your body, and do one small task.
You’ll be surprised how often the urge drops.
What about vaping or “just smoking socially”?
For emphysema prevention, the safest rule is: avoid inhaling anything besides clean air.
“Social smoking” can still turn into regular exposure, and lungs don’t grade on a curve.
If you’re trying to quit and you’re under 18, talk with a trusted adult and a healthcare professional about the safest, most effective options for you.
Tip #2: Dodge lung irritants like they’re spoilers for your favorite show
Lungs are designed for oxygennot a sampler platter of smoke, particles, and chemicals.
Long-term irritation contributes to inflammation and damage.
Emphysema prevention means reducing the total “irritant load” your lungs deal with across years.
At home: Make indoor air boring (in a good way)
- Keep the home smoke-free (including secondhand smoke). “Cracking a window” is not a magical force field.
- Ventilate when cooking: use a range hood that vents outside if possible.
- Be cautious with strong fumes: bleach + ammonia is a hard no; strong cleaners and sprays should be used with ventilation.
- Reduce fine particles: if wildfire smoke or pollution is an issue, consider a HEPA air purifier for the room you sleep in.
- Change HVAC filters on schedule and keep humidity reasonable to limit mold.
Outdoors: Use air-quality strategy, not willpower
On bad air days, it’s not “weak” to adjust your planit’s smart.
Check the Air Quality Index (AQI) and fine particle pollution (PM2.5) alerts when pollution or wildfire smoke is common.
If air quality is poor, shift workouts indoors, shorten outdoor time, and avoid heavy exertion near traffic.
Specific example: If you normally run outside after school or work, keep an indoor backup plan:
a brisk stair walk, a bodyweight routine, or a treadmill session.
Consistency beats “perfect conditions” every time.
At work: Protect your lungs like you protect your paycheck
Occupational exposure to dusts, fumes, vapors, gases, and chemicals is a real COPD/emphysema riskespecially over years.
If your job includes airborne hazards, use the protective controls available:
ventilation, wet-cutting methods (to reduce dust), and properly selected respiratory protection when required.
- Ask what you’re breathing: request the safety data or hazard information for materials you use.
- Use engineering controls (local exhaust ventilation, dust collection) when possible.
- Wear the right protection when requiredand make sure it fits correctly. A respirator that doesn’t seal is basically a face accessory.
- Don’t “tough it out” through chronic cough or wheezeget evaluated.
Tip #3: Prevent respiratory infections (they can speed up lung decline)
Respiratory infections can hit harder in people with COPD risk factors and can worsen breathing problems.
Prevention here is less glamorous than a superhero cape, but more effective:
vaccines, hand hygiene, and early treatment when you’re truly sick.
The vaccine short-list to discuss with a healthcare professional
- Flu vaccine (yearly)
- Pneumococcal vaccines (based on age and risk factors)
- COVID-19 vaccine (per current guidance)
- RSV vaccine (for older adults and certain higher-risk groups)
Add common-sense layers: wash hands, avoid sharing drinks, and consider masking in crowded indoor spaces during respiratory virus seasonespecially if you’re high-risk or around vulnerable people.
If you have frequent infections or lingering cough, don’t “wait it out” forever; get checked.
Tip #4: Build lung reserve with movement (yes, even if you hate cardio)
Regular physical activity supports better breathing efficiency, stronger respiratory muscles, and overall stamina.
Exercise won’t “vaccinate” you against emphysema, but it does improve resilienceespecially if you’re at risk.
A simple weekly structure that protects lung health
- 150 minutes/week of moderate movement (brisk walking counts)
- 2 days/week of strength training (bodyweight is fine)
- Daily breathing breaks: try pursed-lip breathing during stressful moments
If you already have breathing symptoms or early COPD changes, ask about pulmonary rehabilitation.
It’s like physical therapy for your lungsstructured exercise, education, and coaching that can improve how you function day to day.
Tip #5: Eat and sleep like your lungs are on your team (because they are)
No single “superfood” prevents emphysema, but your overall lifestyle can reduce inflammation and support immune function.
Aim for a balanced pattern:
fruits and vegetables, fiber-rich carbs, lean proteins, and healthy fats.
Stay hydrated so mucus stays easier to clear, and prioritize sleep so your body can recover.
Also important: maintain a healthy weight for you.
Being undernourished can weaken muscles (including breathing muscles), while excess weight can make breathing feel harder.
If weight is a struggle, focus on small, sustainable changes rather than extreme plans.
Tip #6: Know your riskespecially the genetic “plot twist” (alpha-1)
Alpha-1 antitrypsin (AAT) deficiency is an inherited condition that raises the risk of COPD/emphysema.
You can’t prevent the genes you inherited, but you can prevent additional lung injury by avoiding smoke and irritantsand you can get tested if you’re at risk.
When to ask about AAT deficiency testing
- Emphysema or COPD at an unusually young age
- Emphysema with little or no smoking history
- A strong family history of COPD/emphysema
- Unexplained breathing symptoms that don’t match your exposure history
Testing is typically done with a blood test, sometimes followed by additional testing to understand severity.
If AAT deficiency runs in your family, earlier awareness can change how carefully you protect your lungs.
Tip #7: Get symptoms checked early (because “it’s probably nothing” is not a plan)
Emphysema and COPD often build quietly.
If you notice persistent cough, shortness of breath with activities that used to feel easy, frequent bronchitis, wheezing, or chest tightness, talk with a healthcare professional.
Testing like spirometry can help identify airflow limitation earlywhen lifestyle changes can have the biggest impact.
Common myths (let’s retire these)
Myth: “Only smokers get emphysema.”
Smoking is the biggest risk factor, but long-term exposure to dusts, fumes, air pollution, and genetics can also contribute.
Prevention should include clean-air habits and workplace protection, not just smoking status.
Myth: “If I quit, my lungs instantly reset.”
Quitting helps immediately in many ways, and it can slow worsening over timebut existing damage doesn’t simply vanish.
That’s not discouraging; it’s empowering: every smoke-free day protects the lung function you still have.
Myth: “I’m young, so I’m safe.”
Lung protection is a long game.
The earlier you reduce exposure to irritants, the more you preserve lung capacity for decades.
Future-you deserves nice thingslike breathing without effort.
A quick emphysema prevention checklist
- Make your home and car smoke-free (no exceptions)
- If you smoke: set a quit date, get support, and use proven tools
- Reduce indoor fumes and improve ventilation (especially when cooking/cleaning)
- Check AQI/PM2.5 during pollution or wildfire smoke seasons
- Use workplace protection for dust/fumes; speak up about safety controls
- Stay updated on recommended vaccines and treat infections early
- Move your body weeklybuild endurance and strength
- Ask about testing if you have strong family history or early symptoms
Bottom line
Emphysema prevention isn’t one magic trickit’s a set of choices that reduce lung irritation and protect your air sacs over time.
The biggest wins come from avoiding smoking (and secondhand smoke), minimizing exposure to pollutants and workplace hazards, preventing respiratory infections, and staying active.
Start with one change you can keep this week, then build.
Your lungs are surprisingly loyal when you stop treating them like a campfire.
Experiences: What emphysema prevention looks like in real life (about )
The advice above can feel abstract until it shows up in daily lifeso here are a few true-to-life “composite” experiences based on common situations people describe.
Names and details are generalized, but the lessons are very real.
1) “I didn’t quit smoking with motivation. I quit with a system.”
One former smoker described realizing that motivation was unreliableespecially on stressful days.
What worked was building a repeatable system: a quit date, removing cigarettes from the house, and swapping the after-dinner smoke with a five-minute walk.
They used nicotine replacement therapy to take the edge off cravings and kept gum in the car because driving was a major trigger.
The biggest surprise? The cravings didn’t vanish, but they became predictableand that made them beatable.
After a few weeks, the person noticed stairs felt less punishing.
It wasn’t a superhero transformation; it was just fewer “bad breathing moments,” which was enough to keep going.
2) “My job wasn’t the problemmy unprotected lungs were.”
A construction worker talked about years of “just dealing with dust.”
The wake-up call wasn’t dramatic; it was annoying: a cough that wouldn’t leave and a wheeze that showed up at night.
They started treating lung protection like any other safety rulehard hat, boots, and the correct respiratory protection when needed.
They also got more serious about ventilation and dust control instead of relying on “it’ll settle eventually.”
The big change wasn’t only physical; it was social.
Once they asked for safer practices, coworkers followed.
It turned into a team norm, not a personal quirk.
That’s how prevention spreads: one person makes it normal to protect their lungs.
3) “Air quality made my ‘healthy routine’ unhealthyuntil I adjusted.”
Another person loved outdoor runsuntil wildfire smoke seasons became routine.
They felt stubborn at first, running anyway because the sky “didn’t look that bad.”
Then they started checking AQI and PM2.5 alerts.
On poor-air days, they ran indoors, did strength workouts, or walked in the early morning when air tended to be better.
It wasn’t as scenic, but it was sustainable.
The takeaway was simple: protecting lungs sometimes means protecting routines from the environment.
Consistent exercise supports lung health, but only if you’re not inhaling a cloud of fine particles while doing it.
4) “Family history changed how I treated ‘little symptoms.’”
Someone with relatives who had COPD said they used to ignore mild shortness of breath because it felt “too small to matter.”
Once they learned about genetic risk (including alpha-1 in some families), they took symptoms seriously.
They asked a healthcare professional about testing and got spirometry to establish a baseline.
They didn’t panic; they planned.
They became strict about secondhand smoke exposure, updated vaccines, and kept indoor air cleaner.
The biggest benefit wasn’t a single test resultit was clarity.
When you understand your risk, you stop negotiating with harmful exposures.
Prevention becomes less about fear and more about protecting your future capacity to do normal, joyful thingswalks, travel, playing with kids, singing in the car without getting winded.







