Table of Contents >> Show >> Hide
- What Are Menopausal Hot Flashes, Exactly?
- The Big Questions Everyone Asks
- Q4: Are hot flashes dangerous, or just miserable?
- Q5: What tends to trigger hot flashes?
- Q6: Is hormone therapy really the most effective treatment?
- Q7: If I still have a uterus, do I need progesterone with estrogen?
- Q8: What if I can’t or don’t want to use hormones?
- Q9: What about newer prescriptions for hot flashes?
- Q10: Do supplements and “natural” remedies work?
- Q11: Can lifestyle changes really help?
- Q12: When should I call a doctor soon?
- An Expert’s Step-by-Step Relief Plan
- Myth-Busting in 90 Seconds
- Conclusion: You’re Not Overreacting, and You’re Not Out of Options
- Experience Section: Real-World Menopausal Hot Flash Stories (Extended)
If your body has recently decided to turn into a space heater at random momentsduring meetings, in traffic, at 2:17 a.m., or right as you finally get comfortable under a blanketyou are absolutely not alone.
Menopausal hot flashes are one of the most common symptoms of the menopause transition, and they can feel anywhere from mildly annoying to “Why am I sweating in a freezer aisle?”
In this expert-style Q&A guide, we’ll break down what hot flashes are, why they happen, what helps, what’s hype, and how to build a practical relief plan that fits your real life.
No scare tactics. No magical mystery teas. Just smart, evidence-based strategies with enough humor to make this topic easier to live with.
What Are Menopausal Hot Flashes, Exactly?
Q1: What does a hot flash feel like?
A hot flash is a sudden wave of heatoften in the face, neck, and chestfollowed by sweating, flushing, and sometimes chills as your body cools down.
Some episodes last under a minute; others linger longer and can leave you feeling drained, damp, and mildly offended.
If these episodes happen during sleep, they’re called night sweats, and they can seriously disrupt rest. That sleep disruption then creates a chain reaction: fatigue, irritability, brain fog, sugar cravings, and the famous “Why did I walk into this room?” feeling.
Q2: Why do hot flashes happen during menopause?
During perimenopause and menopause, estrogen and progesterone levels fluctuate and eventually decline.
Those hormonal shifts affect the brain’s temperature control network (particularly in the hypothalamus), making your internal thermostat more reactive.
In plain English: tiny changes in body temperature that never used to bother you can now trigger a full “all systems overheat” event.
Q3: When do they start, and how long do they last?
Hot flashes can begin in perimenopause (before your final period), continue through menopause, and sometimes last for years afterward.
Menopause itself is officially confirmed after 12 consecutive months without a menstrual period.
Duration varies. Some women have symptoms for a shorter window; others continue for many years.
That range is normal. If yours have lasted longer than expected, you’re not “doing menopause wrong”you’re within the broad spectrum clinicians see every day.
The Big Questions Everyone Asks
Q4: Are hot flashes dangerous, or just miserable?
For most women, hot flashes are not dangerous, but they can be very disruptive to quality of lifesleep, work performance, mood, confidence, and relationships.
They’re especially frustrating when they arrive during presentations, social events, or any moment requiring composure and dry clothing.
Persistent symptoms are worth treating. You do not have to “just tough it out.”
If hot flashes are affecting your daily function, that is reason enough to discuss treatment options.
Q5: What tends to trigger hot flashes?
Common triggers include:
- Warm rooms and heavy bedding
- Alcohol (especially red wine for some people)
- Caffeine
- Spicy foods
- Stress and anxiety spikes
- Smoking
- Tight or non-breathable clothing
Important nuance: triggers are personal. Your friend’s “safe” coffee might be your personal volcano button. Track patterns for two to three weeks before making dramatic lifestyle cuts.
Q6: Is hormone therapy really the most effective treatment?
For women who are appropriate candidates, systemic menopausal hormone therapy is generally the most effective treatment for moderate to severe hot flashes and night sweats.
It tends to work better than lifestyle-only approaches when symptoms are intense.
Treatment is individualized: age, time since menopause, personal and family history, cardiovascular risk, clot risk, breast cancer history, migraine profile, liver health, and symptom burden all matter.
This is why one-size-fits-all advice from social media should be treated like expired yogurt.
Q7: If I still have a uterus, do I need progesterone with estrogen?
Often, yes. In many cases, women with an intact uterus need progestogen alongside systemic estrogen to protect the uterine lining.
Your clinician chooses the regimen based on your cycle stage (perimenopause vs postmenopause), symptoms, and risk profile.
Q8: What if I can’t or don’t want to use hormones?
You still have options. Nonhormonal strategies include certain prescription medications and structured behavioral approaches.
Depending on your health history, your clinician may discuss:
- Some SSRIs/SNRIs for vasomotor symptom relief
- Gabapentin in select situations
- Other nonhormonal medications based on symptom pattern and tolerability
- Newer neurokinin-targeting medications for hot flashes
- Cognitive behavioral therapy (especially if sleep and stress are major issues)
- Clinical hypnosis in appropriately trained settings
Not every option fits every person, and side effects differ. “Nonhormonal” does not mean “risk-free,” but it does mean there are legitimate alternatives if hormones are not right for you.
Q9: What about newer prescriptions for hot flashes?
Newer nonhormonal prescription options that target the brain’s temperature pathways have expanded treatment choices in recent years.
This is promising for women who cannot use estrogen therapy.
Like any medication class, these treatments require careful review of liver health, other medications, and side effects.
Translation: they are good tools, not vending-machine snacks. A proper medication review is essential.
Q10: Do supplements and “natural” remedies work?
Some women report subjective relief from supplements or herbal products, but evidence is mixed and often inconsistent.
“Natural” is not a synonym for “effective” or “safe,” especially when product quality varies and interactions with prescription medications are possible.
If you want to try a supplement, bring the exact product label to your clinician or pharmacist first.
It’s not being dramatic; it’s being smart and preventing a preventable problem.
Q11: Can lifestyle changes really help?
Yesespecially as part of a layered strategy. Lifestyle changes may not erase severe hot flashes on their own, but they can reduce frequency, intensity, and day-to-day misery:
- Dress in breathable layers you can remove quickly
- Use a bedside fan and moisture-wicking sleepwear
- Keep a cool drink nearby
- Limit late-day caffeine and alcohol if they trigger symptoms
- Practice stress downshifting (paced breathing, short mindfulness breaks)
- Prioritize regular movement and resistance training
- Work toward a healthy weight if clinically appropriate
- Avoid smoking; if you smoke, seek cessation support
Think “systems, not heroics.” Tiny repeatable habits beat giant unsustainable overhauls every time.
Q12: When should I call a doctor soon?
Reach out if:
- Symptoms are disrupting sleep, work, or mental health
- You have bleeding after menopause or unusual bleeding patterns
- You have severe mood changes, persistent insomnia, or cognitive concerns
- You’re considering hormone or nonhormonal prescription therapy
- You have complex medical history (blood clots, cancer history, stroke risk, liver disease)
Seek urgent care for red-flag symptoms like chest pain, shortness of breath, severe one-sided weakness, or sudden neurologic symptomsthose are not standard menopause symptoms and should be evaluated immediately.
An Expert’s Step-by-Step Relief Plan
Step 1: Track your pattern for 14 days
Note time of day, trigger exposure, intensity, and how long episodes last.
Add sleep quality and mood. This creates a map of your symptom ecology and helps avoid random treatment guessing.
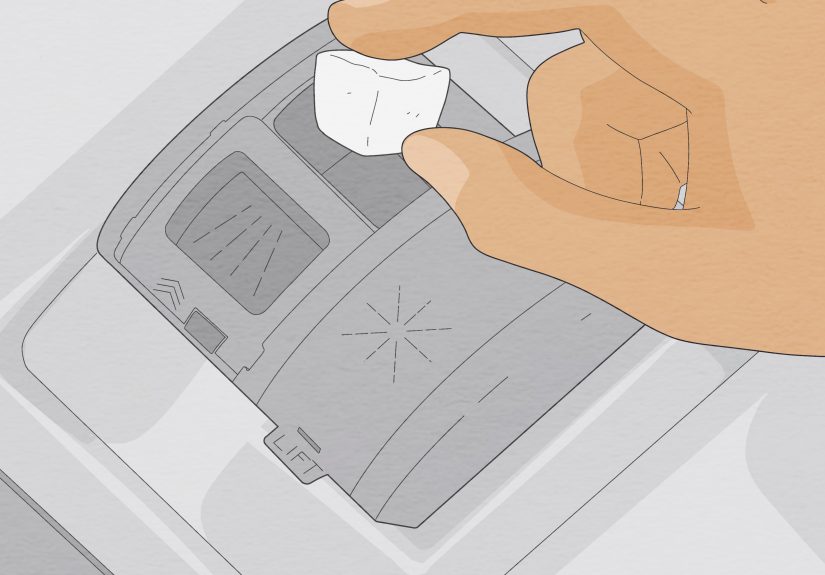
Step 2: Build your “cool-down environment”
Adjust room temperature, bedding, pajamas, and work clothing. Keep cooling tools where symptoms happen most: bedroom, desk, car, gym bag.
Step 3: Treat sleep like a medical priority
Night sweats plus poor sleep can make hot flashes feel worse the next day.
Keep a regular sleep window, reduce evening stimulants, and create a low-heat bedtime routine.
Better sleep won’t cure menopausebut it dramatically improves coping bandwidth.
Step 4: Discuss medical options early, not after burnout
If symptoms are moderate to severe, don’t wait until you’re running on fumes.
A thoughtful visit can clarify whether hormone therapy, nonhormonal medication, or a combined plan makes sense for your health profile and goals.
Step 5: Reassess every few months
Menopausal symptoms change over time. Your treatment plan should too.
The best plan is not the most complicated oneit’s the one you can actually live with.
Myth-Busting in 90 Seconds
- Myth: “Hot flashes are short and harmless, so treatment is unnecessary.”
Reality: They can last years and significantly affect quality of life. - Myth: “If one friend improved on a supplement, it will work for everyone.”
Reality: Responses vary; evidence quality and product consistency matter. - Myth: “Hormone therapy is always unsafe.”
Reality: Risk-benefit depends on timing, health profile, and formulation. - Myth: “Nonhormonal means no side effects.”
Reality: All medications have potential tradeoffs and monitoring needs.
Conclusion: You’re Not Overreacting, and You’re Not Out of Options
Menopausal hot flashes are common, biologically real, and often under-treated.
The good news is that modern care offers more choices than ever: hormonal, nonhormonal, behavioral, and combined approaches.
If your symptoms are mild, smart habit adjustments may be enough. If they’re moderate to severe, targeted medical treatment can be life-changing.
Either way, you deserve a plan based on evidencenot guesswork, guilt, or internet folklore.
And if someone tells you to “just power through,” you can smile politely, adjust your cooling fan, and choose better advice.
Experience Section: Real-World Menopausal Hot Flash Stories (Extended)
The experiences below are composite-style examples based on common patterns clinicians hear from patients. They are not diagnoses, but they are very real in spirit.
1) “The Boardroom Bonfire”
A 49-year-old project manager described her first severe hot flash as “an elevator ride from normal to tropical in eight seconds.”
It happened mid-presentation. She felt heat surge from chest to scalp, then sweat under bright office lights, followed by chills.
What made it worse wasn’t only the symptomit was the fear of it happening again in public.
Her first win came from logistics, not medication: breathable layers, a cold bottle on standby, and choosing a seat near airflow in meetings.
She also reduced late-afternoon coffee and noticed fewer evening episodes. Over time, she worked with her clinician on a treatment plan because night symptoms were still waking her repeatedly.
Her biggest takeaway: “I thought I had to choose between suffering and overreacting. Turns out I could choose a plan.”
2) “The 3 A.M. Pajama Rotation”
A 52-year-old teacher said nights were the hardest part: wake sweaty, change clothes, flip the pillow, fall asleep, repeat.
After weeks of fragmented sleep, her concentration dipped and her patience disappeared. She said, “I wasn’t just tiredI felt like a grumpy ghost of myself.”
Her relief started with sleep triage: moisture-wicking sleepwear, lighter bedding, cooler room temp, and no alcohol close to bedtime.
She added a brief wind-down routine and a consistent bedtime. These changes helped, but not enough.
After discussing options with her clinician, she added targeted therapy, and within weeks she reported fewer awakenings and better daytime energy.
Her phrase was perfect: “I didn’t need perfection. I needed my nights back.”
3) “The Fitness Myth Reset”
A 46-year-old woman in perimenopause assumed that because she exercised regularly, hot flashes wouldn’t hit her hard.
When they did, she blamed herself: wrong workouts, wrong food, wrong routine.
Her clinician helped reframe the issue: fitness supports overall health, mood, and sleep, but it does not immunize anyone against hormonal thermoregulation changes.
She switched from “punishment workouts” to strategic movement: strength training, moderate cardio, recovery days, and hydration discipline.
She tracked triggers and noticed spicy dinners plus red wine created overnight flare-ups.
Cutting those on work nights improved sleep quality. The mindset shift mattered most: “My body wasn’t failing. It was changing. I needed tools, not blame.”
4) “The Quiet Confidence Comeback”
A 55-year-old business owner had frequent daytime flashes plus anxiety about social events. She started declining invitations and avoiding public speaking.
Her confidence took a hit she didn’t expect. In clinic, she said, “I can handle discomfort. What I can’t handle is unpredictability.”
She built a layered plan: trigger awareness, practical cooling prep, stress-regulation techniques, and medical treatment after reviewing her risk profile.
She also told close colleagues what she was managing, which reduced the shame spiral. Instead of hiding symptoms, she normalized them.
Within a few months, she returned to speaking events with fewer episodes and less fear.
Her closing thought deserves to be on a poster: “Menopause didn’t make me less capable. It made me more intentional.”
What These Experiences Have in Common
Different ages. Different careers. Different symptom patterns. Same core lesson: hot flashes are manageable when you combine good information, personalized care, and practical habits.
There is no single “perfect menopause routine,” but there is usually a right-for-you combination that reduces suffering and restores control.
If you remember one thing, let it be this: menopausal hot flashes are common, treatable, and nothing to be embarrassed about.
You are allowed to seek relief early, adjust your plan over time, and prioritize quality of life. That’s not indulgentit’s good medicine.