Table of Contents >> Show >> Hide
- Lymphoma 101: What’s Going Wrong in the First Place?
- Hodgkin vs Non-Hodgkin Lymphoma at a Glance
- Shared and Unique Risk Factors
- Symptoms: Hodgkin vs Non-Hodgkin Lymphoma
- Diagnosis and Staging: How Doctors Tell Them Apart
- Treatment Options for Hodgkin Lymphoma
- Treatment Options for Non-Hodgkin Lymphoma
- Prognosis: How Do Outcomes Compare?
- Questions to Ask Your Cancer Care Team
- Real-World Experiences and Practical Insights
- Bottom Line
Hearing the word “lymphoma” in a doctor’s office can make time stop. Then your brain kicks back in with a million questions:
Is it Hodgkin or non-Hodgkin? Which one is worse? What does treatment look like? Am I going to be okay?
Take a breath. Both Hodgkin lymphoma (HL) and non-Hodgkin lymphoma (NHL) are treatable, and in many cases, highly curable cancers.
Modern therapies are light-years ahead of where they were a few decades ago. This guide breaks down Hodgkin vs non-Hodgkin lymphoma,
what makes them different, how they’re treated, and what real people often experience on the journey.
Quick note: This article is for general education only and doesn’t replace medical advice. Always talk with your oncology team about your specific situation.
Lymphoma 101: What’s Going Wrong in the First Place?
Your lymphatic system is part drainage system, part security team. It includes lymph nodes, spleen, tonsils, bone marrow, and a network of vessels
carrying a clear fluid called lymph. Inside that fluid are lymphocyteswhite blood cells that help your body fight infections.
Lymphoma happens when some of these lymphocytes start growing and dividing in an out-of-control way. Instead of doing their job,
they crowd out healthy cells and form tumors in lymph nodes or other organs.
Doctors generally divide lymphoma into two big families:
- Hodgkin lymphoma (HL)
- Non-Hodgkin lymphoma (NHL)
There are many subtypes, but at a high level, they behave differently, respond to different treatments, and have slightly different outlooks.
Hodgkin vs Non-Hodgkin Lymphoma at a Glance
The “Signature Cell” Difference
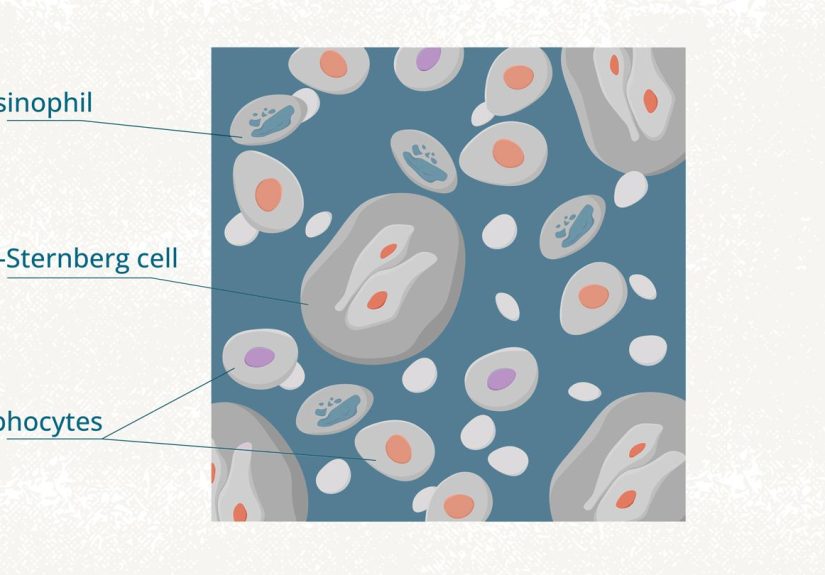
The classic difference has to do with what the cancer looks like under a microscope:
-
Hodgkin lymphoma: Pathologists usually see large, abnormal cells called
Reed–Sternberg cells in the lymph node biopsy. These are like the “calling card” of classical Hodgkin lymphoma. -
Non-Hodgkin lymphoma: No Reed–Sternberg cells. Instead, cells may be abnormal B lymphocytes, T lymphocytes,
or (less often) natural killer (NK) cells.
How Common Are They?
- Non-Hodgkin lymphoma is much more common overall and makes up the majority of lymphoma diagnoses in the United States.
- Hodgkin lymphoma is less common but one of the most curable cancers with modern therapy, especially in younger people.
Who Typically Gets Each Type?
- Hodgkin lymphoma: Often has a “double peak” in agefrequent in teens and young adults, then again later in life. It’s strongly associated with B cells.
- Non-Hodgkin lymphoma: More common as people get older; many cases are diagnosed in people over 60. It includes dozens of subtypes with very different behaviors.
How They Spread and Grow
-
Hodgkin lymphoma tends to spread in an orderly way from one group of lymph nodes to the next.
That predictable pattern makes staging and planning treatment simpler. -
Non-Hodgkin lymphoma can be more unpredictable. Some types are slow-growing (“indolent”), others are fast-growing (“aggressive”),
and spread can skip around the body.
Overall Outlook
Thanks to modern therapy, both Hodgkin and many types of non-Hodgkin lymphoma have very good long-term survival rates.
On average, Hodgkin lymphoma tends to have slightly higher cure rates, but many NHL subtypes are also very treatable.
Shared and Unique Risk Factors
Most of the time, people with lymphoma did nothing to “cause” it. It’s usually a mix of random genetic changes and factors we don’t fully understand.
Still, some trends show up in research:
Risk Factors Seen in Both
- Weakened immune system (for example, after an organ transplant or with HIV)
- Certain autoimmune diseases
- Family history of lymphoma
- Exposure to some chemicals or pesticides (still being studied)
Risk Factors More Linked with Hodgkin Lymphoma
- Previous infection with Epstein–Barr virus (EBV), the virus that can cause mono
- Having a close relative with Hodgkin lymphoma
Risk Factors More Linked with Non-Hodgkin Lymphoma
- Older age
- Certain infections (for example, H. pylori in the stomach or hepatitis C for some subtypes)
- Long-term immune suppression medicines
But again, many people with lymphoma have none of these risk factors. So if you’re tempted to blame yourself, please don’tthis is not a “you ate the wrong snack” kind of disease.
Symptoms: Hodgkin vs Non-Hodgkin Lymphoma
Hodgkin and non-Hodgkin lymphoma often look very similar on the outside. Common signs include:
- Painless swollen lymph nodes in the neck, armpits, or groin
- “B symptoms”: fevers, drenching night sweats, unexplained weight loss
- Extreme tiredness or weakness
- Itchy skin or rash without a clear cause
- Persistent cough, chest pain, or trouble breathing if lymph nodes in the chest are enlarged
- Fullness, discomfort, or pain in the abdomen if the spleen or abdominal lymph nodes are involved
Some people feel basically fine and discover lymphoma after a routine exam or imaging test for something else. Others feel unwell for months without a clear reason.
The only way to know for sure is with proper medical evaluation and usually a lymph node biopsy.
Diagnosis and Staging: How Doctors Tell Them Apart
If lymphoma is suspected, your care team will typically order a series of tests to confirm the diagnosis and stage the disease (how far it has spread).
Key Steps in Diagnosis
- Lymph node biopsy: A surgeon removes all or part of a lymph node. A pathologist examines the tissue under a microscope, looks for Reed–Sternberg cells, and uses special stains to classify the exact type of lymphoma.
- Blood tests: To check blood counts, liver and kidney function, and sometimes markers of inflammation.
- Imaging: CT scans and PET-CT scans help show where lymphoma is in the body and how active it is.
- Bone marrow biopsy: Sometimes needed to see if lymphoma has reached the bone marrow.
Staging (I to IV)
Both Hodgkin and non-Hodgkin lymphomas are staged using a system from I (limited) to IV (more widespread). Doctors also use letters like:
- A – No significant B symptoms
- B – Presence of fever, night sweats, or weight loss
- E – Lymphoma has spread just outside the lymph system
Stage is important, but in lymphoma, type and biology of the cells often matter just as much as how far it has spread.
Treatment Options for Hodgkin Lymphoma
Hodgkin lymphoma is one of the genuine success stories of modern oncology. Today, up to about 9 out of 10 people with newly diagnosed Hodgkin lymphoma
can be cured with combination therapy in high-income countries.
Common Treatments
-
Chemotherapy: Usually given in combinations (regimens) such as ABVD or other modern protocols. These drugs travel through the bloodstream
to kill lymphoma cells throughout the body. -
Radiation therapy: Often used for early-stage disease or to treat specific areas where lymphoma was bulky. Modern techniques try to limit
radiation exposure to healthy organs. -
Targeted therapy and immunotherapy:
Drugs like brentuximab vedotin (which targets a protein called CD30) or immune checkpoint inhibitors may be used in specific situations,
such as relapsed or refractory disease. -
Stem cell (bone marrow) transplant:
For people whose Hodgkin lymphoma returns or doesn’t respond well to initial therapy, high-dose chemotherapy followed by a stem cell transplant
(often using the person’s own cells) can offer another chance at cure.
The exact combination depends on stage, age, other health conditions, and how the lymphoma responds early in treatment (often shown on PET scans).
Treatment Options for Non-Hodgkin Lymphoma
“Non-Hodgkin lymphoma” is really an umbrella label for many different cancers. That means treatment is less one-size-fits-all and more “pick from the menu
based on the subtype.”
Indolent (Slow-Growing) NHL
Examples include follicular lymphoma and some marginal zone lymphomas. These cancers may grow slowly for many years.
-
Watchful waiting (active surveillance): If symptoms are mild and organ function is okay, doctors may monitor with regular exams and scans
rather than start treatment right away. - Immunochemotherapy: Many patients receive combinations of chemotherapy plus monoclonal antibodies like rituximab that target B cells.
- Targeted therapies: Oral drugs that interfere with specific growth signals in lymphoma cells are increasingly used in certain subtypes.
- Radiation therapy: For localized disease or to treat symptoms in a specific area.
Aggressive (Fast-Growing) NHL
The most common aggressive subtype is diffuse large B-cell lymphoma (DLBCL).
These lymphomas grow quickly but are often very responsive to treatment.
-
Combination chemo-immunotherapy:
A standard regimen for many B-cell NHLs is R-CHOPa mix of chemotherapy drugs plus rituximab, given in cycles. - Radiation therapy: Sometimes added to treat bulky areas or residual disease.
- Stem cell transplant: For relapsed disease, high-dose chemotherapy and autologous (your own) stem cell transplant may be recommended.
-
CAR T-cell therapy and newer options: For some people whose lymphoma comes back after multiple treatments,
engineered immune cells called CAR T cells or new antibody-based therapies can be used at specialized centers.
T-cell NHLs and rarer subtypes have their own specific protocols. That’s why getting care from a team with lymphoma expertise is so important.
Prognosis: How Do Outcomes Compare?
It’s natural to ask, “What’s my chance of beating this?” While every person is different, large databases give us some big-picture trends:
- Hodgkin lymphoma: Overall 5-year relative survival in the U.S. is close to 90%, and even higher in some early-stage groups.
-
Non-Hodgkin lymphoma: Average 5-year survival is a bit lower than Hodgkin lymphoma, but still strong overall.
Some subtypes have excellent long-term outcomes; others are more challenging but still increasingly treatable.
Factors that influence prognosis include:
- Exact subtype of lymphoma
- Stage and presence of B symptoms
- Age and general health
- How well the cancer responds to the first rounds of treatment
The takeaway: whether it’s Hodgkin or non-Hodgkin, the label is just one piece of the puzzle. Modern therapy, clinical trials, and supportive care can dramatically shape the story.
Questions to Ask Your Cancer Care Team
When you’re comparing Hodgkin vs non-Hodgkin lymphoma, the most important part is how your specific diagnosis will be handled.
Consider asking:
- What exact type of lymphoma do I have? Is it Hodgkin or non-Hodgkin, and which subtype?
- What stage is my lymphoma, and what does that mean in practical terms?
- What treatment options do you recommend first, and why?
- Are there clinical trials that might be appropriate for me?
- What are the most common side effects of this treatment, and how do we manage them?
- How will treatment affect my fertility, work, family life, and daily routine?
- What does follow-up care look like after treatment?
Bringing a written list, a friend or family member, and a notebook (or notes app) can make these conversations less overwhelming.
Real-World Experiences and Practical Insights
Every lymphoma story is unique, but many people with Hodgkin or non-Hodgkin lymphoma move through similar emotional and practical phases.
The details here are drawn from common themes in patient stories, not any single person’s experience.
From “What Is That Lump?” to Diagnosis
Imagine you’re in the shower one morning and feel a firm, painless lump above your collarbone. It doesn’t hurt, so you ignore it for a while.
Weeks later, it’s still thereand now you’re feeling unusually wiped out. Eventually, your primary care provider orders blood tests, then a scan,
then a biopsy. Suddenly you’re in an oncologist’s office hearing the words “Hodgkin lymphoma” or “diffuse large B-cell lymphoma.”
Many people describe this phase as a blur of appointments, acronyms, and Google searches at 2 a.m. One of the most helpful things during this time is
having someone you trust come to appointments to take notes and help process information. Another is giving yourself permission to ask the same question
more than oncedoctors expect that, and good teams don’t mind repeating themselves.
Navigating Treatment: Chemo, Radiation, and All the Logistics
Treatment for Hodgkin and non-Hodgkin lymphoma can be intense, but it’s usually time-limited and designed with a clear goal.
People often say that having a planfor example, six cycles of chemo, followed by a scan and maybe radiationhelps them feel more in control.
Day-to-day, there are many small strategies that make a big difference:
-
Managing side effects:
Anti-nausea meds, staying hydrated, and communicating early about symptoms like fevers or severe fatigue can keep treatment on track. -
Energy budgeting:
Some people use a “spoon theory” approachtreating energy like a limited daily budget and spending it wisely on essentials and a few things that bring joy. -
Support network:
Friends and family often want to help but don’t know how. Specific requestsrides to chemo, help with meals, child care, or just company during infusion
can turn vague offers into real support. -
Work and finances:
Social workers and patient navigators can help with disability paperwork, workplace accommodations, and financial aid programs for treatment costs.
For some people with more aggressive NHL or relapsed Hodgkin lymphoma, the journey includes high-dose chemo and a stem cell transplant.
That can mean a longer hospital stay and a heavier recovery period, but many survivors describe this as the step that gave them their life back.
Emotional Ups and Downs
One of the most surprising parts of lymphoma, whether Hodgkin or non-Hodgkin, is how emotionally uneven the ride can be:
- Shock and fear at diagnosis
- Determination when treatment starts (“Let’s do this.”)
- Frustration on rough days or when plans get delayed by low blood counts or infections
- Mixed feelings after treatmentrelief plus anxiety about scans, long-term effects, or recurrence
Many people find counseling, support groups, or online communities helpful, especially when friends and family don’t fully understand what “scanxiety”
feels like. Talking with others who’ve had Hodgkin or non-Hodgkin lymphoma can turn medical jargon into real-world wisdomthings like which snacks sit
well on chemo days, or how they handled hair loss, or what made the long hours in infusion chairs more bearable.
Life After Treatment: A New Normal
When active treatment ends, the world expects you to celebrate and “get back to normal.” But for many lymphoma survivors, this part can be surprisingly complicated.
You may look healthy on the outside while still dealing with fatigue, brain fog, or the emotional whiplash of what you’ve just lived through.
Follow-up visits and scans are typically spaced out over months and then years. During this time, people often:
- Pay more attention to sleep, nutrition, and movementnot as magic cures, but as tools for healing.
- Learn to balance staying vigilant about symptoms with not living in constant fear.
- Reassess priorities: work, relationships, hobbies, and what feels truly important.
Whether your diagnosis is Hodgkin or non-Hodgkin lymphoma, it’s very possible to move into a long-term survivor role.
Many people eventually find themselves mentoring newly diagnosed patients, answering the same questions they once asked:
“What does chemo feel like?” “Will my hair grow back?” “How did you handle the waiting?” In that way, lymphoma journeys become a chain of shared knowledge and hope.
Bottom Line
Hodgkin vs non-Hodgkin lymphoma isn’t really a battle where one is “good” and the other is “bad.” They’re different diseases with different biology,
different standard treatments, and somewhat different typical age groups. But both are treatable, and many people with either diagnosis
go on to live long, full lives.
The most important step is partnering with a knowledgeable oncology team, understanding your specific subtype and stage, and asking every question you need
to feel informed. Statistics describe groups; your story is your ownand with modern care, there is very real reason for hope.







