Table of Contents >> Show >> Hide
- A quick IUD refresher (because context helps)
- Copper vs. hormonal IUD: side effect cheat sheet
- Common IUD side effects (and what’s “normal”)
- Less common but important risks (rare, but know the signs)
- How to manage IUD side effects (practical, real-life strategies)
- When to call a clinician right away
- Tips that can make insertion and the first week easier
- If side effects don’t improve: what are your options?
- FAQ (because your brain will ask these at 2 a.m.)
- of real-world “experience” (what it can feel like, and how people handle it)
- Conclusion
Getting an IUD can feel a little like hiring a tiny, T-shaped bouncer for your uterus: it shows up, takes its job very seriously,
and occasionally makes its presence known with a few strongly worded “notes” (read: cramps, spotting, or a surprise plot twist in your period).
The good news? Most IUD side effects are common, expected, and manageableespecially in the first few months while your body adjusts.
This guide breaks down what side effects you might notice, which ones are more common with copper vs. hormonal IUDs,
what you can do at home to feel better, and when it’s time to call a clinician. (Because peace of mind is also a form of healthcare.)
A quick IUD refresher (because context helps)
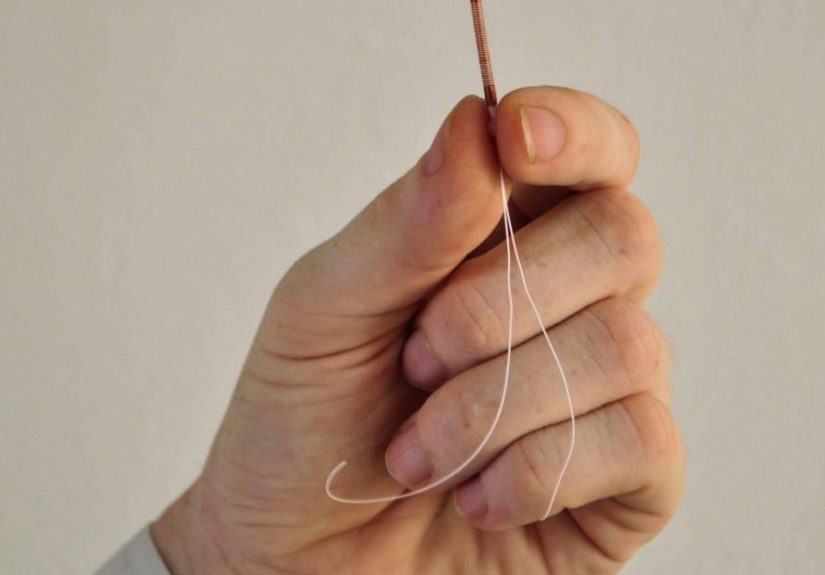
An intrauterine device (IUD) is a small device placed in the uterus by a healthcare professional to prevent pregnancy.
There are two main types:
- Copper IUD (non-hormonal): uses copper to interfere with sperm function. Periods may be heavier at first.
- Hormonal IUD (progestin/levonorgestrel): releases a small amount of progestin locally in the uterus. Bleeding often becomes lighter over time, and some people stop having periods.
Both are highly effective and long-acting, but their side effect “personalities” can be differentlike siblings raised in the same house
who still somehow turned out wildly opposite.
Copper vs. hormonal IUD: side effect cheat sheet
| Side effect | More common with copper IUD | More common with hormonal IUD |
|---|---|---|
| Heavier/longer periods (early months) | Yes | Less likely |
| More cramps during periods (early months) | Yes | Sometimes (often improves) |
| Spotting/irregular bleeding | Possible | Common early on |
| Lighter periods or no periods | No | Yes (can happen over time) |
| Hormone-type symptoms (acne, headaches, breast tenderness, mood changes) | No (since no hormones) | Possible (usually mild) |
Common IUD side effects (and what’s “normal”)
1) Cramping and pelvic pain
Mild to moderate cramping is one of the most common side effects, especially right after insertion and during the first few cycles.
Think “period cramps with opinions.” Some people feel fine the same day; others feel crampy for a few days.
In the first 3–6 months, cramping can show up around your period as your uterus adjusts.
What helps: heat (heating pad or warm bath), rest, gentle movement, and over-the-counter pain relievers if they’re safe for you.
Many clinicians recommend an anti-inflammatory option (like ibuprofen or naproxen) because it helps with cramping caused by uterine prostaglandins.
If you’re under 18, have stomach/kidney issues, take blood thinners, or aren’t sure what’s safeask a clinician or pharmacist first.
2) Spotting and irregular bleeding
Spotting (light bleeding between periods) is especially common in the first few months, particularly with hormonal IUDs.
Your uterus lining is adapting, and it sometimes responds like a roommate rearranging furniture at 2 a.m.annoying, but usually temporary.
What helps: track it (so you can see improvement over time), wear liners you actually like, and give it a little time.
If bleeding becomes very heavy, lasts a long time without improving, or comes with significant pain, it’s worth checking in with your provider.
3) Heavier periods (copper IUD)
The copper IUD can cause heavier, longer, or more crampy periodsmost commonly in the first 3–6 months.
For many people, this eases with time. But if you already have very heavy periods, anemia, or a bleeding disorder,
this is an important “talk it through” point before choosing copper.
What helps: anti-inflammatory pain relievers (if safe), heat, hydration, and iron-rich foods if you’re losing more blood than usual.
If you’re soaking through pads/tampons quickly, passing large clots, feeling dizzy, or getting short of breath, call a clinician promptly.
4) Lighter periodsor no periods (hormonal IUD)
Many people have lighter periods over time with a hormonal IUD, and some stop bleeding altogether.
This can be a welcome surprise (“My period ghosted me”)and it’s typically a normal effect of the uterine lining becoming thinner.
If you suddenly stop having periods after they were regular with the IUD, or you have pregnancy symptoms,
take a pregnancy test and contact your clinician for guidance.
5) Hormone-adjacent symptoms (hormonal IUD)
Hormonal IUDs release progestin mostly in the uterus, but some people still notice symptoms such as acne, headaches,
breast tenderness, nausea, or mood changesespecially early on. These are usually mild and often improve as your body settles in.
- Acne: gentle cleanser, non-comedogenic moisturizer, and spot treatments (like benzoyl peroxide) can help. If it’s persistent, a clinician can suggest prescription options.
- Headaches: hydrate, eat regular meals, sleep consistently, and use OTC pain relief if safe. New severe headaches should be checked.
- Mood changes: keep a simple symptom log. If you feel persistently down, anxious, or unlike yourself, talk to a trusted adult and a healthcare professionalthere are options and you don’t have to “push through.”
6) Backaches, dizziness, or feeling “off” right after insertion
Some people feel lightheaded, sweaty, or dizzy during or right after insertion (a vagal response).
It’s not a character flaw; it’s your nervous system being dramatic. Clinics are used to this and can help you rest and recover.
What helps: eat something beforehand if your clinician says it’s okay, hydrate, plan a low-key day, and consider having someone drive you home.
7) Ovarian cysts (usually harmless)
Functional ovarian cysts can occur in some hormonal IUD users. Most are benign and go away on their own.
Sometimes they cause one-sided pelvic discomfort, bloating, or a “twinge” feeling.
If pain is sudden, severe, or comes with fever, vomiting, or fainting, get urgent medical evaluation.
Less common but important risks (rare, but know the signs)
Serious complications are uncommon, but it’s smart to know what they look likekind of like knowing where the fire extinguisher is.
You hope you never need it, but you sleep better knowing it’s there.
1) Expulsion (the IUD partially or fully slips out)
Expulsion is most likely in the first months after insertion. Sometimes you’ll notice longer strings,
feel the hard plastic at the cervix, or have a sudden return to your pre-IUD bleeding/cramping pattern.
Sometimes you won’t feel anything at all.
What to do: use backup contraception and contact your clinician if you suspect expulsion.
If you can’t feel the strings (or they suddenly feel much longer/shorter), your provider can check placement.
2) Infection / pelvic inflammatory disease (PID)
The overall risk is low, but the risk of PID is highest shortly after insertion, especially if someone has an untreated STI at the time of placement.
Symptoms to watch for include fever, chills, worsening pelvic pain, unusual or foul-smelling discharge, or pain during sex.
What to do: call a clinician urgentlyprompt evaluation and treatment matter.
3) Perforation (very rare)
Perforation means the IUD goes through the uterine wall during insertion. It’s rare, but it can happen.
Severe pain that doesn’t improve, heavy bleeding, or pain that gets worsenot bettershould be evaluated.
4) Pregnancy with an IUD in place (uncommon, but urgent to assess)
IUDs are very effective, but no method is perfect. If you think you might be pregnant (missed period with symptoms, positive test),
contact your clinician promptly. Any pregnancy with an IUD needs evaluation to rule out ectopic pregnancy (a pregnancy outside the uterus),
which can be dangerous.
How to manage IUD side effects (practical, real-life strategies)
Pain and cramping game plan
- Heat: heating pad on the lower abdomen or back for 15–20 minutes at a time.
- Movement: gentle walking, stretching, or yoga can reduce muscle tension and improve blood flow.
- Anti-inflammatory meds: if safe for you, they can help cramps and sometimes bleeding. Follow the label or your clinician’s instructions.
- Schedule smart: if possible, plan insertion before a lighter daynot right before a major exam, a long flight, or your friend’s “standing-room-only” concert.
Bleeding and spotting sanity savers
- Track patterns: use an app or notes: days of bleeding, intensity, and symptoms. This helps you see progress and gives your clinician useful info.
- Give it a window: many people see improvement by 3–6 months (earlier for some, later for others).
- Build iron habits: if bleeding is heavier, focus on iron-rich foods (lean meats, beans, lentils, spinach) plus vitamin C to help absorption.
- Ask about options: if heavy bleeding is persistent, a clinician may offer treatments (sometimes short-term meds) or discuss switching IUD types.
Hormonal symptom tweaks (if they show up)
- Skin: keep it simplecleanser, moisturizer, sunscreen. Add acne treatments slowly so you don’t irritate your skin.
- Headaches: steady sleep, hydration, regular meals. New severe headaches deserve medical advice.
- Mood: symptom tracking, stress support, and talking to a professional if symptoms are persistent or intense.
When to call a clinician right away
Contact a healthcare professional urgently (same day if possible) if you have:
- Severe pelvic or abdominal pain, especially if it’s worsening or not improving
- Fever, chills, or flu-like symptoms after insertion
- Foul-smelling or unusual discharge
- Very heavy bleeding (for example, soaking through a pad/tampon quickly or feeling dizzy/weak)
- A positive pregnancy test or strong pregnancy symptoms
- Strings suddenly much longer/shorter, you can feel plastic at the cervix, or you suspect expulsion
Tips that can make insertion and the first week easier
- Eat and hydrate ahead of time (unless your clinic instructs otherwise).
- Ask about pain control options: OTC meds beforehand (if safe), local numbing, or other clinic strategies.
- Plan recovery time: comfy clothes, heating pad, easy meals, and permission to do absolutely nothing impressive for 24 hours.
- Bring support if you cansomeone to drive you or hang out afterward can make the day feel less intense.
If side effects don’t improve: what are your options?
If you’re past the adjustment window (often around 3–6 months) and side effects still feel like they’re running your life,
you have choices:
- Check placement: sometimes an ultrasound or exam is used to confirm the IUD is positioned correctly.
- Treat the symptom: a clinician may recommend short-term treatment for bleeding or pain.
- Switch types: if copper causes heavy periods, a hormonal IUD may help; if hormones bother you, copper might be better.
- Remove it: removal is typically quick in a clinic. Your provider can help you choose another method that fits your body and your life.
FAQ (because your brain will ask these at 2 a.m.)
Do IUDs protect against STIs?
No. If STI protection matters for you, condoms (internal or external) are a helpful add-on. Dual protection is not overachieving;
it’s just smart.
Can I check my IUD strings?
Many people can feel the strings high in the vagina with clean fingers. Your clinician can explain how and when to check.
If you can’t feel them (or they feel very different), don’t panicjust contact your provider for guidance.
Will my partner feel the IUD during sex?
Usually no. Sometimes a partner feels the strings early on; strings often soften and curl over time.
If it’s uncomfortable, a clinician may be able to adjust string length.
of real-world “experience” (what it can feel like, and how people handle it)
Scenario 1: The “Is this normal?” week.
A lot of people describe the first day or two after insertion as “period cramps, but with extra attitude.”
The most common move is a heating pad, a comfy couch setup, and the kind of TV that doesn’t require emotional labor.
By day three, many feel noticeably betterstill crampy here and there, but functional. The biggest relief often comes from
realizing that the sensation isn’t getting worse; it’s gradually fading. The best tip people share? Plan insertion like you’d plan a minor storm:
stock snacks, clear your schedule, and make peace with sweatpants as formalwear.
Scenario 2: The spotting saga.
Spotting can be the side effect that tests your patience, because it’s not dramatic enough to feel “urgent” but persistent enough to feel rude.
People often say it helps to track itbecause in your head it feels like “forever,” but the calendar usually shows it’s trending downward.
Many switch to liners they actually like, keep spare underwear around (adulting!), and set a mental checkpoint:
“If this isn’t improving by month three, I’ll message my clinician.” That plan turns vague anxiety into a timeline,
and timelines are basically anxiety’s natural predator.
Scenario 3: Copper IUD + heavy periods = negotiation time.
Some copper IUD users notice heavier periods early on and feel like they’re suddenly starring in a very unfun historical drama called
“The Crimson Tide.” A common approach is using anti-inflammatory pain relief (if safe), heating pads, and being extra mindful about iron.
People who do best often build a “heavy day kit”: preferred period products, backup clothes, and a water bottle.
Many report it improves after a few cycles, but they also emphasize this: if you’re soaking through products quickly or feeling weak/dizzy,
don’t tough it out. Getting checked isn’t “complaining,” it’s making sure you’re safe.
Scenario 4: Hormonal IUD surprises (lighter periods, mood blips, or acne).
A hormonal IUD can feel like a choose-your-own-adventure book: some people get lighter periods and think, “Wow, love this for me.”
Others get a few months of unpredictable spotting, mild headaches, or skin changes. The real-world strategy many share is staying consistent
with basicssleep, hydration, mealsand keeping skincare gentle rather than throwing every product at your face at once.
For mood changes, people often say the turning point is talking about it sooner: with a clinician, therapist, or trusted adult.
Even if the IUD isn’t the cause, you deserve support. And if it is the cause, you have optionsswitching methods is allowed.
Your birth control should fit your life, not the other way around.
Conclusion
IUD side effects can be annoying, but most are temporary and manageableespecially during the first few months.
The key is knowing what’s typical (cramps, spotting, bleeding changes), using practical tools to feel better,
and recognizing red-flag symptoms that deserve prompt medical attention. If your side effects aren’t improving
or don’t feel acceptable to you, that’s validand there are plenty of options, including switching IUD types or choosing a different method.






