Table of Contents >> Show >> Hide
- What is prednisone, exactly?
- What is prednisone used for?
- Prednisone dosage: the practical framework
- Prednisone side effects: common, serious, and long-term
- Drug interactions and precautions
- Special populations: extra caution, smarter monitoring
- How to take prednisone more safely: a practical checklist
- When to call your healthcare team now (not later)
- 500-word experience section: real-life prednisone journeys and lessons learned
- Experience 1: “I felt better in 24 hours, so I stopped.”
- Experience 2: “Why am I awake at 3 a.m. reorganizing my pantry?”
- Experience 3: “My glucose numbers went wild.”
- Experience 4: “I ignored swelling and blood pressure until my shoes disagreed.”
- Experience 5: “I thought side effects meant treatment failure.”
- Conclusion
- SEO Tags
If medications had personalities, prednisone would be the “gets-things-done” friend who shows up with a toolbox, a checklist, and maybe a tiny bit too much energy. It can calm inflammation fast, reduce immune overreactions, and help people get through flares that would otherwise derail daily life. But it is also a medicine that deserves respect: the same power that helps can cause side effects when dose, timing, or duration are off.
In this guide, you’ll get a practical, in-depth look at prednisone uses, dosage principles, common and serious side effects, interaction red flags, and real-world tips that make treatment safer and easier to follow. You’ll also find a long experience section at the end with realistic patient-style scenarios and what they teach us. This article is educational, not a personal prescriptionyour own clinician should make final dosing decisions.
What is prednisone, exactly?
Prednisone is an oral corticosteroid (a glucocorticoid) used to reduce inflammation and suppress an overactive immune response. It is often described as a “prodrug,” meaning your body converts it (mainly in the liver) into prednisolone, the active form that does most of the heavy lifting.
Clinically, prednisone can be used as anti-inflammatory therapy, immunosuppressive therapy, or steroid replacement in certain endocrine conditions. In plain English: it helps when your immune system is too loud, your inflammation is too intense, or your body is not producing enough steroid hormone naturally.
What is prednisone used for?
Prednisone has broad indications across multiple specialties. That doesn’t mean it is first choice for every case, but it remains a cornerstone medication in many care plans.
Common use categories
- Respiratory conditions: asthma exacerbations, selected COPD flare settings, severe airway inflammation.
- Allergic and dermatologic diseases: severe allergic reactions, severe eczema/dermatitis patterns, inflammatory skin disorders.
- Rheumatologic and autoimmune conditions: rheumatoid arthritis flares, lupus activity, vasculitic and inflammatory syndromes.
- Gastrointestinal inflammatory disease: short-term control of inflammatory bowel disease flares in selected patients.
- Hematologic/oncologic and other conditions: specific protocols where immunosuppression or anti-inflammatory effect is needed.
- Adrenal/endocrine indications: steroid replacement in certain adrenal insufficiency scenarios.
One reason prednisone is prescribed so frequently is speed: it can suppress flare symptoms quickly. Another reason is flexibility: clinicians can tailor dose intensity, schedule, and taper length based on disease severity, treatment history, and risk profile.
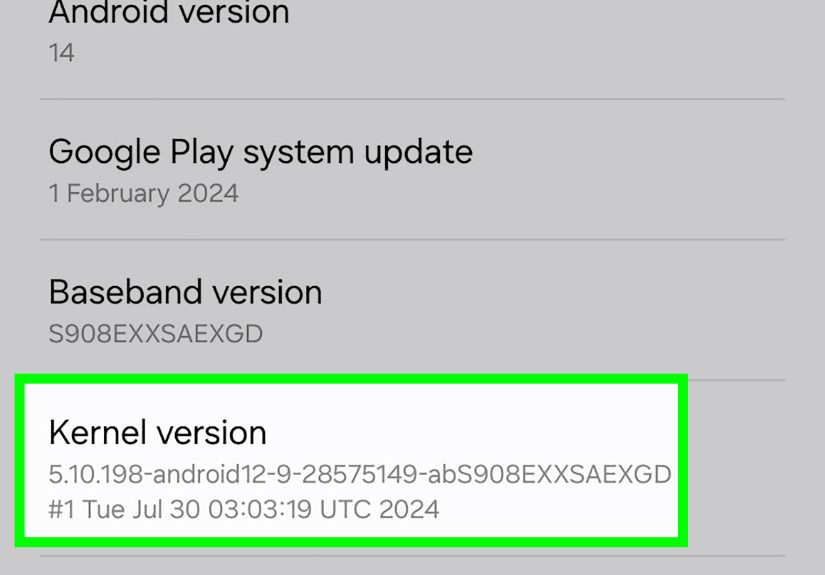
Prednisone dosage: the practical framework
There is no one-size-fits-all prednisone dose. If you ever hear someone say, “Everyone should take exactly X mg,” that’s your cue to run the opposite direction (politely). Dosing depends on diagnosis, severity, age, comorbidities, and treatment goals.
Typical dosing principles
- Initial daily dose range can vary widely: in labeling contexts, adult starts may range from low doses to much higher short-course doses depending on condition.
- Use the lowest effective dose: clinicians often adjust quickly once control is achieved.
- Prefer morning dosing when once daily: often improves alignment with natural steroid rhythms and may reduce certain side effects.
- Take with food (or milk if advised): can reduce stomach irritation.
- Duration matters as much as dose: a brief burst and a long-term regimen are very different risk situations.
Simple dosing examples (educational only, not a prescription)
| Clinical pattern | Typical approach | Main goal |
|---|---|---|
| Short, acute flare | Higher short-term dose, then taper | Fast control of inflammation |
| Moderate ongoing inflammation | Lowest effective daily dose, reassess frequently | Control symptoms while minimizing side effects |
| Longer-term autoimmune plan | Bridge strategy while slower long-term meds begin working | Maintain function, reduce flare burden |
| Adrenal replacement context | Physiologic replacement schedule per endocrinology plan | Hormone replacement, not high-dose immunosuppression |
Why tapering matters
If prednisone has been used long enough (or at high enough doses), stopping suddenly can cause steroid withdrawal and adrenal insufficiency symptoms such as severe fatigue, weakness, nausea/upset stomach, and blood-pressure-related symptoms. Tapering allows your adrenal system time to wake back up.
Translation: don’t “freestyle” your steroid stop plan. If your prescription changes, follow the taper exactly and ask for written instructions.
Prednisone side effects: common, serious, and long-term
Side effects are dose- and time-dependent: higher dose plus longer duration generally increases risk. Not everyone experiences major problems, but everyone should know what to monitor.
Common short-term side effects
- Increased appetite and possible weight gain
- Trouble sleeping (especially when taken late in the day)
- Mood shifts (irritability, restlessness, feeling “wired”)
- Indigestion or stomach upset
- Fluid retention/puffiness
- Headache or mild dizziness
- Acne or skin changes
Serious side effects that need urgent medical attention
- Signs of infection: fever, chills, persistent sore throat, worsening cough, non-healing wounds
- Severe mood or behavior changes, confusion, or major depression symptoms
- Vision changes, eye pain, or sudden visual blurring
- Black/tarry stools, vomiting blood, or severe abdominal pain (possible GI bleeding)
- Marked high blood sugar symptoms: unusual thirst, frequent urination, unexplained fatigue
- Severe swelling, shortness of breath, or concerning blood-pressure changes
Long-term risks to discuss early
- Bone loss/osteoporosis and fractures (risk rises with ongoing steroid exposure)
- Hyperglycemia/diabetes worsening
- Hypertension and fluid retention
- Cataracts and glaucoma risk
- Muscle weakness and slower wound healing
- Increased infection susceptibility
- Adrenal suppression with abrupt discontinuation risk
Think of prednisone side effects like sunlight exposure: one short walk is usually manageable; unprotected all-day exposure every day is a different story. Dose, duration, and prevention strategies change the outcome.
Drug interactions and precautions
Prednisone has many potential interactions. Always share a complete medication list, including supplements and herbals.
Interaction categories to watch closely
- NSAIDs (like ibuprofen/naproxen): may increase GI irritation/bleeding risk when combined in some patients.
- Warfarin and other anticoagulants: response can shift; closer monitoring may be needed.
- Diabetes medications: prednisone can raise blood glucose, requiring medication adjustments.
- CYP3A4-related interactions: certain medications can increase or reduce steroid exposure.
- Vaccines: live vaccines may be contraindicated or delayed at immunosuppressive steroid doses.
- Herbal products/supplements: some can alter metabolism or side-effect risk.
Vaccine timing and prednisone
For people on high-dose systemic prednisone for long enough duration, live vaccines are often deferred for a period after therapy. Lower-dose or short-course therapy may not carry the same restriction. The key point is timing and dose intensity, so ask your clinician before any vaccination during steroid treatment.
Special populations: extra caution, smarter monitoring
Children and teens
Long-term systemic steroid exposure may affect growth and bone health. Pediatric plans should include close follow-up, growth tracking, and the shortest effective steroid exposure.
People with diabetes or prediabetes
Prednisone can raise blood sugar quickly. People on insulin or oral diabetes meds may need short-term dose changes and more frequent glucose checks during bursts.
People with osteoporosis risk
If steroid exposure is ongoing, discuss bone protection early: calcium/vitamin D intake, weight-bearing activity, smoking cessation, fall prevention, and whether bone-density testing or additional therapy is appropriate.
People with infection risk or immune compromise
Prednisone can mask infection signs while also lowering immune defense. That combination can delay diagnosis if people wait too long to report symptoms.
Pregnancy and breastfeeding context
Prednisone decisions during pregnancy or lactation are individualized risk-benefit choices. In many cases, clinicians still use steroids when disease control is crucial; the safest plan is condition-specific and coordinated with obstetric and specialty care.
How to take prednisone more safely: a practical checklist
- Take exactly as prescribed; do not self-adjust unless your clinician tells you to.
- Prefer morning dose timing if once daily and approved in your plan.
- Take with food to reduce stomach irritation.
- Track daily symptoms: sleep, mood, swelling, appetite, blood pressure, blood sugar (if applicable).
- Use a written taper calendar; check off each dose.
- Report infection signs early; don’t “wait it out” when immunosuppressed.
- Review vaccine timing before shots.
- Bring a full medication/supplement list to every visit.
- Discuss bone protection if treatment extends beyond short bursts.
- Keep follow-up appointments for labs and monitoring.
Tiny habits prevent big headaches. Prednisone can be a very effective medicine when monitored intentionally rather than casually.
When to call your healthcare team now (not later)
- Fever, persistent sore throat, or signs of a spreading infection
- Severe mood changes, agitation, confusion, or significant depressive symptoms
- Vision changes or eye pain
- Black stools, vomiting blood, or severe abdominal pain
- Marked swelling, shortness of breath, or chest symptoms
- Severe weakness after dose reduction or abrupt missed doses
If symptoms are severe or rapidly worsening, seek emergency care. Fast action beats internet searching at 2:00 a.m.
500-word experience section: real-life prednisone journeys and lessons learned
The following are composite, educational experiences based on common clinical patternsnot individual medical records. They’re included to make this topic practical, relatable, and easier to remember.
Experience 1: “I felt better in 24 hours, so I stopped.”
A patient with a bad inflammatory flare started feeling dramatically better after the first day and decided the medication had “done its job.” They skipped the rest of the taper. Two days later: crushing fatigue, body aches, nausea, and dizziness. They thought the original illness had returned, but the bigger issue was abrupt steroid withdrawal after their body had already started adapting. Once they restarted under clinician guidance and tapered correctly, symptoms settled. Lesson: improvement is not the finish line; taper completion is part of treatment. Prednisone can feel like a sprint, but the safe ending is usually a controlled jog, not a cliff jump.
Experience 2: “Why am I awake at 3 a.m. reorganizing my pantry?”
Another person took prednisone in the evening because “that’s when I remembered.” Within days they reported racing thoughts, poor sleep, and irritability. The dose itself was reasonable, but timing amplified side effects. Their clinician shifted the dose to morning with breakfast and added a few sleep hygiene rules: no late caffeine, consistent bedtime, and no revenge-scroll marathons. Sleep improved within several nights, and mood stabilized. Lesson: timing can change tolerance dramatically. The same milligrams can feel very different at 8 a.m. versus 8 p.m.
Experience 3: “My glucose numbers went wild.”
A patient with type 2 diabetes started a prednisone burst for a respiratory flare. Their blood sugar climbed quickly, even though they had been stable for months. Instead of panicking, they contacted their care team early, adjusted diabetes meds temporarily, increased glucose checks, and used a lower-carb meal plan during treatment. After the steroid course ended, numbers trended back toward baseline. Lesson: this is common and manageable with proactive monitoring. If you have diabetes or prediabetes, think “plan first, react less.”
Experience 4: “I ignored swelling and blood pressure until my shoes disagreed.”
One long-course user noticed ankle swelling and tighter rings but assumed it was “just summer.” A routine check revealed elevated blood pressure. Their clinician adjusted dose strategy, tightened sodium intake, and monitored labs and vitals more closely. Symptoms improved, and no emergency developed. Lesson: fluid retention is not just cosmetic. Home blood pressure checks, sodium awareness, and early reporting can prevent bigger complications.
Experience 5: “I thought side effects meant treatment failure.”
A patient on a moderate course developed acne, appetite increase, and mood swings and felt discouraged“If this medicine is working, why do I feel weird?” Their clinician reframed the situation: side effects do not automatically mean failure; they are signals to optimize dose, duration, timing, and supportive care. They switched to the lowest effective dose sooner, added structured meals, protected sleep, and built a taper calendar. Symptoms became manageable, disease control held, and confidence returned. Lesson: successful prednisone therapy is rarely passive. It’s an active collaboration with adjustments, check-ins, and honest symptom tracking.
Across these experiences, one theme repeats: people do best when they treat prednisone like a precision tool, not a casual pain reliever. Ask questions early, write instructions down, and make monitoring part of the plan. When used thoughtfully, prednisone can be the bridge that gets you from chaos back to functionwithout unnecessary detours.
Conclusion
Prednisone remains one of the most effective anti-inflammatory and immunosuppressive oral medicines in routine practice. It can work quickly, cover a wide range of conditions, and stabilize difficult flares when used correctly. But it is not “set and forget.” Dose personalization, morning timing, taper discipline, interaction checks, and side-effect monitoring are the difference between a helpful course and a complicated one.
If you remember just one thing: prednisone is safest when you and your care team run it as a plan, not an improvisation.