Table of Contents >> Show >> Hide
- The “Nodule” Moment: What Doctors Mean
- Does a Prostate Nodule Mean Cancer?
- Common Noncancer Causes That Can Feel Like a Nodule
- How Doctors Work Up a Prostate Nodule (The Practical Playbook)
- If It Is Cancer: What Happens Next?
- When to Get Checked (Sooner, Not Later)
- Quick FAQ
- Real-World Experiences: What This Journey Often Feels Like (500+ Words)
- Conclusion
Educational content only. If you’ve been told you have a prostate nodule, talk with a qualified clinicianpreferably a urologistfor personalized advice.
Few phrases can turn a routine checkup into a full-blown Google spiral faster than “I felt a nodule on your prostate”.
It’s right up there with “we should run a few tests” and “please don’t eat before your appointment”short, ominous, and annoyingly vague.
But here’s the honest truth: a prostate nodule is not automatically cancer. It’s a clue. A flag. A “hey, we should look closer.”
Sometimes that closer look finds prostate cancer. Often it finds something elselike inflammation, benign enlargement, or calcifications (tiny deposits that can feel firm).
This article breaks down what a prostate nodule can mean, what doctors do next, and how to keep your sanity while your lab results take their sweet time
getting back to you.
The “Nodule” Moment: What Doctors Mean
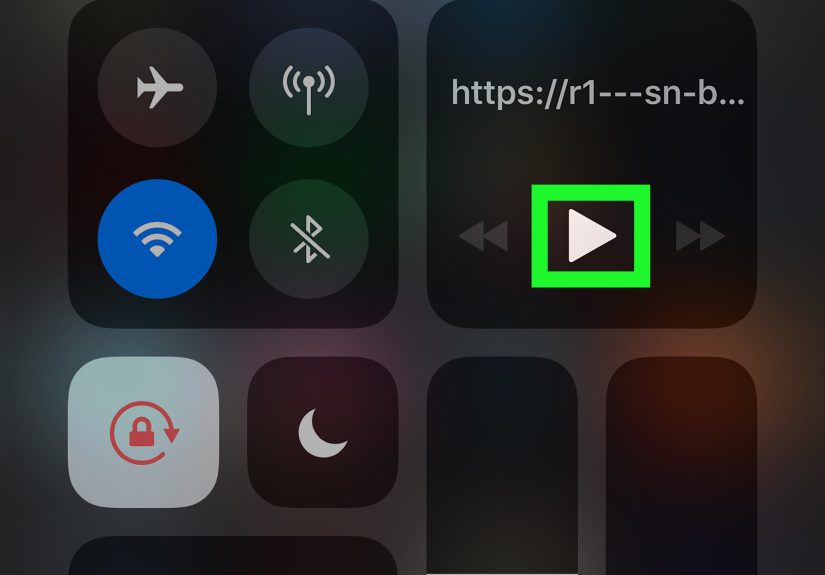
Most prostate nodules are discovered during a digital rectal exam (DRE)a quick exam where a clinician feels the back surface of the prostate through the rectum.
In real-world terms: it’s a gloved finger, a little lubricant, and about 10 seconds of you staring at the ceiling and contemplating your life choices.
During a DRE, the clinician is checking whether the prostate feels:
- Symmetric or uneven
- Soft or unusually firm
- Smooth or irregular
- Tender (which can hint at inflammation)
A “nodule” generally means a firm or raised area that feels different from the rest of the gland. The key point: the DRE can only assess
part of the prostate, and “feels different” does not equal “definitely malignant.” It simply means the prostate isn’t reading from the standard script.
Does a Prostate Nodule Mean Cancer?
A prostate nodule can be associated with prostate cancer, but it can also reflect benign conditions. Clinicians take nodules seriously because
prostate cancer can present as a firm area on the glandespecially when the cancer is near the back portion that a DRE can reach.
That said, many prostate cancers are not felt on DRE, and not every firm area is cancer.
The nodule is best thought of as a starting point for risk assessment. The next steps usually consider:
- Your age and overall health
- Your PSA level and how it has changed over time
- Your symptoms (urinary changes, pelvic pain, blood in urine, etc.)
- Your risk factors (family history, genetics, race/ethnicity, prior biopsy results)
- Whether imaging like multiparametric MRI suggests suspicious areas
If you’re hoping for a single magical number or one definitive exam that settles everything, I’m sorrymedicine rarely respects our desire for tidy endings.
But the good news is that modern evaluation is far more nuanced than “nodule = panic.”
Common Noncancer Causes That Can Feel Like a Nodule
1) Prostatitis (Inflammation or Infection)
Prostatitis is inflammation of the prostate and can be intensely uncomfortableor sneakily subtle. It may cause pelvic pain, burning with urination,
urinary frequency, difficulty urinating, or even flu-like symptoms in acute bacterial cases. Inflammation can make areas of the prostate feel firm, swollen,
or tender on exam, and it can also raise PSA levels.
One tricky thing: prostatitis can mimic cancer in the sense that it can create alarming symptoms and suspicious test results. The difference is that inflammation
often improves with appropriate treatment and time (depending on type), while cancer requires its own workup and management.
2) Benign Prostatic Hyperplasia (BPH)
BPH is benign enlargement of the prostate, and it becomes more common with age. While BPH is often described as “enlargement,” it can also
make the gland feel irregular or bulkythe prostate equivalent of a sweater that shrank in the wash and now fits strangely in the shoulders.
BPH commonly causes urinary symptoms: weak stream, hesitancy, frequent urination, nocturia (getting up at night), and the feeling that the bladder doesn’t empty
completely. BPH can also raise PSA levels because PSA is produced by prostate tissuemore tissue can mean more PSA, even when there’s no cancer.
3) Prostatic Calcifications (Stones/Deposits)
Small calcium deposits can form in the prostate (sometimes called prostatic calculi). These can be incidental findings on imaging, but they can also feel firm
and occasionally contribute to symptoms. Importantly, calcifications themselves aren’t automatically a cancer sign. They can be related to aging, inflammation,
or prior infection. Still, if a firm area is felt on exam, it deserves appropriate evaluation rather than assumptions.
4) Scarring, Cysts, or Post-Inflammatory Changes
Past inflammation can leave fibrosis (scar-like firmness). Cysts can also occur in or near the prostate and may feel like an abnormality
depending on size and location. These are usually benign, but the only responsible approach is to interpret them alongside PSA trends, imaging, andwhen indicatedbiopsy.
5) “False Alarm” Anatomy
Sometimes what feels like a nodule is influenced by exam limitations, stool in the rectum, patient tension, or the simple fact that human anatomy
doesn’t always match the diagrams in textbooks. This is one reason clinicians often confirm findings with repeat exams or imaging rather than
making sweeping conclusions from a single moment.
How Doctors Work Up a Prostate Nodule (The Practical Playbook)
Step 1: History and Symptom Check
Expect questions about urinary symptoms (urgency, frequency, weak stream, nighttime urination), pain, fever/chills, blood in urine or semen,
and recent activities that can affect PSA (like ejaculation, cycling, or recent procedures). Your clinician is trying to sort out whether this looks more like
inflammation, benign enlargement, or something requiring more aggressive evaluation.
Step 2: PSA TestingUseful, Not Perfect
The prostate-specific antigen (PSA) test measures PSA in the blood. PSA can rise with prostate cancer, but also with BPH, prostatitis,
recent ejaculation, vigorous cycling, and even recent prostate manipulation or biopsy. That’s why PSA is best interpreted as a trend and a
contextual clue, not a verdict.
Some clinicians recommend repeating a newly elevated PSA before jumping to advanced testingespecially if there’s a plausible temporary reason for elevation
(like infection or recent ejaculation). This can prevent unnecessary stress and unnecessary procedures.
Step 3: Risk Factors Matter More Than People Think
Clinicians weigh personal risk factors because they change the odds. The most commonly discussed include:
- Age: risk rises as men get older.
- Family history: having a close relative with prostate cancer increases risk.
- Race/ethnicity: in the U.S., Black/African American men have higher risk of developing and dying from prostate cancer.
- Genetic factors: certain inherited mutations (such as harmful BRCA2 changes) raise prostate cancer risk.
None of these mean “you definitely have cancer.” They mean “we choose the next steps more carefully.”
Step 4: Biomarkers and “Second-Layer” Tests (Sometimes)
If PSA is borderline or confusing, clinicians may use additional tests in some settings, such as percent-free PSA or other biomarker panels.
Not everyone needs these, but they can help refine risk when the picture is fuzzy.
Step 5: Multiparametric MRIThe Modern Detective
A multiparametric prostate MRI (mpMRI) can identify suspicious areas and help guide a targeted biopsy. This is a big deal because random
sampling can miss clinically significant cancers, and MRI-targeting can improve detection of cancers that matter most.
MRI isn’t perfectsome cancers don’t show clearly, and not every MRI “suspicious spot” turns out to be cancerbut it often improves decision-making:
who should get biopsied, and where to sample.
Step 6: BiopsyThe Only Way to Confirm Cancer
If concern remains after PSA, DRE, risk factors, and/or MRI, a prostate biopsy may be recommended. A biopsy removes small tissue samples
so a pathologist can look for cancer cells under a microscope.
Biopsies can be done using ultrasound guidance and may be transrectal or transperineal (approach depends on practice and patient factors).
Common short-term side effects can include blood in urine or semen, mild discomfort, and temporary urinary symptoms. Infections are uncommon but important
to watch foryour clinician will advise you on warning signs and prevention steps.
If It Is Cancer: What Happens Next?
If a biopsy finds prostate cancer, the next step is figuring out how aggressive it is and whether it appears confined to the prostate.
Prostate cancer is often graded by patterns seen under the microscope (commonly summarized using Gleason scoring and Grade Groups).
Low-risk disease may not need immediate treatment
Many prostate cancers grow slowly. For men with low-risk disease, one common option is active surveillancecareful monitoring with repeat PSA tests,
imaging, and sometimes repeat biopsies. This approach aims to avoid or delay treatment side effects while still catching progression early.
Higher-risk disease may need active treatment
For cancers that appear more aggressive or more extensive, treatment options may include surgery (prostatectomy), radiation therapy, hormone therapy, or
combinations. The “right” choice depends on cancer features, age, health, and personal priorities (like balancing cure rates with potential urinary or sexual side effects).
The important takeaway: a nodule is not a diagnosis. Even a cancer diagnosis isn’t a single storylineprostate cancer ranges from “watch it carefully”
to “treat it promptly,” and modern care is built around matching the response to the risk.
When to Get Checked (Sooner, Not Later)
A prostate nodule should be evaluated, but it doesn’t require midnight doom-scrolling. Call a clinician promptlyespecially if you have:
- Blood in urine
- Significant trouble urinating or urinary retention
- Fever, chills, or severe pelvic pain (possible infection)
- Rapidly rising PSA levels (if known)
- Strong family history or known genetic risk
If you’re waiting for results, focus on what you can control: follow instructions (like avoiding ejaculation before a PSA test if advised), write down your symptoms,
and prepare questions for your urology visit. Your anxiety wants to “solve” it instantly; medicine prefers evidence.
Quick FAQ
Can a benign nodule raise PSA?
Yes. PSA can rise from benign enlargement (BPH), inflammation (prostatitis), and other noncancer causes. That’s why PSA interpretation depends on the whole clinical picture.
What if my PSA is normal but a nodule is felt?
A normal PSA reduces the odds of significant cancer but doesn’t eliminate it. A suspicious DRE finding may still lead to further evaluation,
such as repeat PSA testing, MRI, or biopsy depending on risk factors and clinician judgment.
Does a biopsy always find cancer if cancer is present?
Biopsy is the standard diagnostic test, but no test is flawless. Sampling can miss a small cancer.
That’s why follow-up matters if suspicion remains, PSA continues to rise, or imaging suggests a target that wasn’t sampled previously.
Is the DRE outdated?
DRE has limitations and is not a standalone screening tool. However, it can still provide useful informationespecially when combined with PSA, risk factors,
and modern tools like mpMRI. Think of it as one clue, not the whole detective novel.
Real-World Experiences: What This Journey Often Feels Like (500+ Words)
Medical explanations are helpful, but they don’t capture the emotional reality of hearing the word “nodule.” In clinics, a few patterns show up again and again
not as identical stories, but as familiar arcs. Here are common experiences people report (shared here as composite examples, not individual patient accounts),
and what they often learn along the way.
1) The “One Weird PSA Spike” Whiplash
A lot of men discover the nodule conversation because of a PSA result that jumps unexpectedly. The emotional experience is usually the same:
“It was fine before… so what changed?” Sometimes, the plot twist is surprisingly ordinaryan infection, inflammation, or even timing.
Men often describe feeling frustrated when they learn that a PSA test isn’t a yes-or-no cancer meter. But many also feel relieved when the clinician says,
“Let’s repeat it under calmer conditions,” because it turns the situation from a cliffhanger into a plan.
One practical takeaway men commonly share: they wish they’d known earlier that temporary factors can affect PSA. It doesn’t mean the test is useless;
it means it’s a tool that behaves better when used thoughtfully.
2) The “Prostatitis Is a Drama Queen” Episode
When prostatitis is involved, people often describe a mix of urinary symptoms and discomfort that feels both personal and disruptive.
They may experience pelvic pressure, burning, urgency, or a sense that their bladder has suddenly developed a grudge.
Being told there’s a firm area on the prostate can feel terrifyinguntil treatment and time start to improve symptoms, and follow-up testing looks less ominous.
Emotionally, this experience often swings between fear (“what if it’s cancer?”) and annoyance (“why didn’t anyone tell me inflammation could mimic this?”).
Many say the most helpful thing was a clinician who explained the “why” in plain English and didn’t dismiss their anxiety.
3) The “MRI Saved Me From Guesswork” Moment
Men who undergo multiparametric MRI often describe it as the point where things start to feel less vague. Before imaging, it’s easy to feel stuck in
ambiguous territory: a nodule was felt, PSA is borderline, and your imagination has moved into your spare bedroom.
MRI can’t promise certainty, but it can add structureidentifying a suspicious target, suggesting a low-risk picture, or helping guide whether a biopsy makes sense.
Many men say the MRI step was psychologically helpful because it created a “map.” Even when the MRI shows something suspicious, it often feels better than
living in an information vacuum.
4) The “Biopsy: Not Fun, But Not the Apocalypse” Reality Check
People tend to dread biopsy. Understandably. But men who’ve gone through it often report a similar conclusion: it was uncomfortable and awkward,
but it was manageableand the clarity afterward was worth it.
The waiting period for results is usually described as the hardest part, because your brain runs simulations without permission.
If the biopsy is negative, many men feel immediate relieffollowed by confusion when the clinician still recommends monitoring.
That follow-up plan can feel counterintuitive until it’s explained: a negative biopsy lowers concern, but continued PSA trends or MRI findings may still warrant observation.
5) The “If It’s Cancer, It’s Not One-Size-Fits-All” Reframe
Men diagnosed with prostate cancer often describe initial shock, then a steep learning curve. The most common surprise:
not everyone needs immediate aggressive treatment. Some cancers are low-risk and monitored, while others require timely treatment.
Many say that once they understood grading (how aggressive the cells look) and staging (where the cancer seems to be), they felt more grounded.
The overarching experience is this: the word “nodule” starts as a jump scare, but with a structured evaluationPSA context, risk factors, MRI, and biopsy when needed
it becomes a problem you can face with information instead of fear.
Conclusion
A prostate nodule is a signal, not a sentence. It can be associated with prostate cancer, but it can also come from common, treatable, noncancer causes like
prostatitis, BPH, and calcifications. The right next steps depend on the whole pictureyour PSA pattern, symptoms, risk factors, and (in many cases) imaging.
If you’ve been told you have a prostate nodule, the best move is simple: don’t ignore it, and don’t catastrophize it.
Get a thoughtful evaluation, ask good questions, and let evidencerather than anxietydrive the next chapter.